Definition... Peptic ulcer disease (PUD) is a chronic recurrent disease in which ulcers form in the gastroduodenal zone due to an imbalance in the physiological balance between aggressive and protective factors. This is one of the most common diseases of the digestive system, 50% of patients in the gastroenterology department in the city hospital are patients with ulcerative lesions of the stomach or duodenal ulcer.
According to US statistics, 25 million patients annually complain of pain in the epigastric region, a decrease in the quality of life due to peptic ulcer disease, 5-10% get sick all their lives, 27-38% have episodes of dangerous bleeding during the first year after an exacerbation, 6500 deaths are recorded outcomes.
In the last quarter of the 20th century, medical tactics for peptic ulcer disease were radically changed due to the study of the molecular mechanisms of acid production and its regulation, the development of new classes of drugs, primarily antisecretory drugs, the discovery Helicobacter pylori(H. pylori), which made it possible to improve the quality of life of a patient with peptic ulcer disease.
Peptic ulcer disease ranks second after chronic gastritis in gastroenterological practice. Men suffer 2 times more often than women. In 80% of cases, people under 40 suffer, which is of great social importance. Over the past 10 years, the previously characteristic seasonality has become blurred.
Peptic ulcer classification based on the following features: localization, etiology, clinical stage.
By localization
Process stage
Complications: bleeding, perforation, perivisceritis, pyloric stenosis, malignancy, penetration
Concomitant diseases of the stomach and duodenum 12
Symptomatic ulcers
Etiology and pathogenesis. PU is a multifactorial disease. Not the disease itself is inherited, but only a predisposition to it (hereditary factors), which is realized under adverse influences (environmental factors). The role of hereditary predisposition is undeniable, especially with pyloroduodenal localization. Duodenal ulcers occur mainly at a young age. Stomach ulcers - in the older.
The risk factors for ulcer include:
a hereditary increase in the mass of parietal cells, their hypersensitivity to gastrin, an increase in the formation of pepsinogen-1 (α1-antitrypsin deficiency) and gastroduodenal motility disorders can lead to damage to the mucous membrane of the stomach and duodenum;
congenital deficiency of mucoproteins of mucus, insufficient production of secreted Ig A and prostaglandins reduce the resistance of the mucous membrane of the stomach and duodenum;
blood group 0 (1), positive Rh factor, the presence of HLA antigens B5, B 15, B35, etc. increase the likelihood of ulcerative disease.
Adverse environmental factors include:
psycho-emotional stress, gross errors in nutrition, bad habits (smoking, alcohol abuse). Food that stimulates the active secretion of gastric juice can have a damaging effect on the gastric mucosa. These are spicy, spicy, smoked foods, fresh baked goods (pies, pancakes), a large amount of food, most likely hot and cold food, irregular meals, dry food, refined foods, excessive consumption of coffee. Normally, mucosal injuries heal in 5 days. The direct ulcerogenic effect of alcohol (weak alcoholic beverages) has not been proven, although it has a powerful sokogenic effect and does not have an antacid effect. Strong alcoholic drinks have a damaging, cauterizing effect.
H. pylori infection and nonsteroidal anti-inflammatory drugs. At present, it is these factors that are assigned the leading role in the realization of hereditary susceptibility to ulcer.
With a combination of hereditary and environmental risk factors, an imbalance develops between the factors of "aggression" and the factors of "protection" of the mucous membrane of the stomach and duodenum, which is a decisive link in the pathogenesis of ulcer.
The factors of aggression include:
violation of the motor-evacuation function of the stomach and duodenum (delay or acceleration of the evacuation of acidic contents from the stomach, duodenogastric reflux);
increased exposure to acid-peptic factor associated with an increase in the production of hydrochloric acid and pepsin;
In connection with big role acid-peptic factor, the classic formula of the early XX century "no acid - no ulcer" has not lost its relevance.
The secretion of hydrochloric acid by the gastric mucosa is provided by parietal (parietal) cells located in the epithelial layer gastric glands fundic department, occurs under the action of secretogens: histamine, gastrin and acetylcholine due to the activation of H 2 -, gastrin and M-cholinergic receptors.
A multicomponent transport system is involved in the penetration of hydrochloric acid through the apical membrane. The main element of this system is the proton pump, which provides ATP-dependent exchange of intracellular H + ions for extracellular K + ions. The role of the proton pump in the system providing the secretion of hydrochloric acid is played by the enzyme - H +, K + -ATPase.
Under the influence of external and internal factors, there is a violation of the coordinating function of the cerebral cortex in relation to the subcortical formations. This causes a secondary persistent excitation of the vagus nuclei. Increasing the tone of the vagus nerves stimulates the secretion of hydrochloric acid, pepsin, and also enhances gastric motility. Vagotonia due to increased activity of the parasympathetic nervous system, It has great importance in the pathogenesis of peptic ulcer disease. Patients often show clinical signs of increased vagus tone: bradycardia, sweating, constipation, etc.
Also important is the effect of local hormones that stimulate the secretion of HCl - an increase in the content or sensitivity to gastrin, histamine, serotonin and inhibiting the secretion of HCl - intestinal peptides (VIP, GIP), somatostatin.
Pepsin is not a primary damaging agent. According to most researchers, it has an effect on the mucous membrane previously damaged by hydrochloric acid.
In the mechanism of ulceration, in addition to the aggressiveness of the environment, the duration of contact of acidic gastric contents with the mucous membrane of one or another part of the gastroduodenal region plays a significant role. Disorders of gastroduodenal motility are directly influenced by the neurohumoral system of the body. If there is a prolonged retention of the contents in the stomach, conditions are created for the development of gastric ulcers, on the contrary, with an intense intake of acidic contents from the stomach into the duodenum or a delay in evacuation along it due to duodenostasis, ulcers are formed in this department.
Duodenogastric reflux occurs due to discoordination of the motor function of the duodenum and stomach against the background of weakness of the pylorus. With duodenogastric reflux, bile acids and lysolecithin enter the stomach. Under their influence, the barrier function of the mucous membrane is disrupted, the reverse diffusion of hydrogen ions is enhanced, which leads to local tissue acidosis and tissue necrosis with the formation of an ulcer.
The normal mucous membrane of the stomach and duodenum is quite resistant to the action of damaging factors. Therefore, in the pathogenesis, it is also necessary to take into account the protective mechanisms that protect the mucous membrane from the formation of ulcers. In the presence of etiological factors, the ulcer is not formed in everyone.
Protection factors include:
resistance of the mucous membrane to aggressive effects;
gastric mucus formation;
adequate bicarbonate production;
active regeneration of the surface epithelium of the mucous membrane;
sufficient blood supply to the mucous membrane;
normal content of prostaglandins in the wall of the mucous membrane;
immune protection.
It is customary to distinguish two components of the protective mucous barrier: a layer of visible, insoluble mucus (first line of defense) and a layer of mucosal epithelial cells (second line of defense).
Visible mucus (mucin) covers the entire mucous membrane of the stomach and duodenum with a thin layer of 1-1.5 mm. Mucus is tightly bound to the surface epithelium by colloidal strands. The composition of mucus is determined by two groups of substances: mucopolysaccharides and glycoproteins, which form complex high molecular weight structures that form a gel. The viscosity and the ability of visible mucus to resist the digestive properties of gastric juice is provided with the participation of fucoglycoproteins and N-acetylneuraminic acid, which belongs to the group of sialomucins.
With a peptic ulcer, the total production of mucus may decrease or its qualitative composition may change. One of the reasons for the development of peptic ulcer disease may be genetically determined features of fucoglycoproteins, which impede their secretion.
The next anatomical substrate of the protective barrier is the cells of the superficial epithelium of the mucous membrane. The stability of the mucous membrane of the stomach and duodenum largely depends on the integrity and adequate regeneration of the apical membrane of cells.
Active regeneration of the superficial epithelium is considered one of the important elements, providing a sufficiently high resistance of the mucous membrane, and if it is damaged, the defect heals quickly. Chronic gastritis, which is based on dysregenerative disorders, in this regard, can contribute to the development of peptic ulcer disease.
In the mucous membrane of the gastroduodenal zone, physicochemical processes constantly occur, which prevent the reverse diffusion of hydrogen ions. Along with the carboxyl groups of mucus glycoproteins, bicarbonate secretion is of great importance in neutralizing H + - ions. Normal secretion of bicarbonates and mucus allows maintaining the pH on the surface of epithelial cells at 7.1-7.4 at a parietal pH of 1.4-2.0. A decrease in the secretion of bicarbonate from the gastric mucosa may play an important role in the formation of gastric ulcers. In the pathogenesis of duodenal ulcer, one should take into account the possibility of reducing the production of pancreatic bicarbonates and "acidification" of the duodenal contents
The role of the vascular component in the development of gastroduo-duodenal ulcers (Virchow's theory) is confirmed by the following facts:
change blood vessels in the ulcer zone (sclerotic lesions of terminal arterioles, their obliteration, dilatation of veins and capillaries);
the frequency of development of peptic ulcer disease in persons with severe stenosis of the celiac trunk and with specific changes in the vessels of the submucosal layer, characteristic of hypertension and diabetes mellitus, many times higher than the average incidence of peptic ulcer disease;
the results of experimental studies showing that ischemia has a significant effect on the state of the protective mucous barrier;
good effect of hyperbaric oxygenation in the treatment of peptic ulcer disease.
In some types of symptomatic gastroduodenal ulcers, the leading role of vascular lesions is obvious. So, microcirculation disorders in the mucous membrane are the main pathogenetic link of stress ulcers, lesions of regional arteries - senile ulcers, specific changes in the vessels of the submucosal layer - ulcers in hypertension.
Currently, the role of prostaglandins and immune disorders in the pathogenesis of peptic ulcer disease is being actively studied.
Prostaglandins are biologically active substances and are derivatives of fatty acids. Clinical and experimental observations have shown that prostaglandins have an antiulcer effect and can prevent the development of gastroduodenal ulceration when exposed to alcohol, salicylates, indomethacin, glucocorticoid drugs.
The most studied mechanism of action of group E2 prostaglandins. Prostaglandins suppress the secretory function of the stomach, increasing the secretion of bicarbonates and mucose, have a cytoprotective effect in doses insufficient to suppress the secretion. The latter effect is associated with an increase in the production of bicarbonates and mucus by the gastric mucosa, as well as with the formation of surfactant-like compounds (phospholipids) by epithelial cells of the stomach and normalization of blood flow in mucose microvessels. Group E prostaglandins have a trophic effect on the mucous membrane of the stomach and duodenum, preventing damage to glandular cells and structural disintegration of mucose.
Recent studies have shown that a variety of immune shifts are observed in peptic ulcer disease. Damaged tissue in the area of the ulcer can eventually acquire the properties of an autoantigen, which is a source of autoaggression and leads to the progression of the disease. In patients with peptic ulcer, a deficiency of secretory immunoglobulin A, which performs a protective function against the mucous membranes, was found. Most likely, immune disorders are secondary, caused by inflammatory changes in the gastric mucosa.
The balance between the factors of aggression of gastric juice and protection of the mucous membrane of the stomach and duodenum in different phases of digestion under changing conditions of the external and internal environment of the body is maintained by the coordinated interaction of the neuroendocrine system. Violations of the integration and coordination functions of this system can play an important role in the pathogenesis of peptic ulcer disease.
The neuroendocrine system that regulates various functions digestive organs, include the parasympathetic link of the autonomic nervous system; sympathetic-adrenal system; system hypothalamus - pituitary gland - peripheral endocrine glands and gastrointestinal hormones. The central place in this system belongs to the hypothalamic region. The cerebral cortex realizes its influence through the hypothalamus, which, however, does not mean constant interference of the cortex in its function; cortical influence is included only in extreme, extreme situations. V normal conditions the hypothalamus constantly monitors and corrects the activity of the endocrine glands and the autonomic nervous system. It has now been established that there is self-regulation of tissue and cellular levels (protein synthesis by the cell, transport of electrolytes and water, cell energetics, etc.), closed self-regulation systems, for example, gastroduodenal, afferent connections of these systems with the higher parts of the central nervous system with the presence of feedback ...
The discovery of gastrointestinal hormones - peptides that control various functions of the gastrointestinal tract - is rightfully considered one of the greatest achievements in biology in recent years. By 1985. 21 types of endocrine gastrointestinal cells were discovered. Their total number is enormous, the mass significantly exceeds the mass of any endocrine gland. Endocrine cells are localized mainly around the nerve endings and vessels of the mucous membrane, which suggests a neuroendocrine complex. The close relationship and mutual influence nervous and hormonal regulatory systems is indicated by the detection of certain peptide hormones of the gastrointestinal tract (gastrin, bombesin, vasoactive intestinal polypeptide) in the structures of the brain, and, conversely, hormones first discovered in brain cells (somatostatin, neurotensin, substance P, enkephalins), as well as pituitary hormones are found in endocrine cells and nerve fibers of the gastrointestinal tract.
Gastrointestinal hormones have a wide spectrum of action on various functions of the stomach and duodenum, violations of which can be of no small importance in the pathogenesis of peptic ulcer disease. Polypeptide hormones stimulate (gastrin, bombesin) or inhibit (somatostatin, vasoactive intestinal peptide, gastric inhibitory peptide) the production of hydrochloric acid, excite (secretin, substance P) or suppress (somatostatin, neurotensin) the active motor secretion of pancreatic bicarbonate activity of the gastrointestinal tract (motilin), increase the production of gastric mucus (somatostatin, bombesin), increase blood flow and regenerative processes in the gastric mucosa (gastrin).
Hormones that increase the activity of the acid-peptic factor: cortisol, T3, T4, insulin, parathyroid hormone, gastrointestinal hormones gastrin, bombesin, neuropeptide R.
Hormones that inhibit gastric secretion: somatostatin, glucagon, sex hormones, calcitonin, gastrointestinal hormones secretin, pancreosimin, enterogastron, gastric inhibitory polypeptide, vasoactive intestinal polypeptide, enkephalins, endorphins.
In 1984, a report was published on the discovery of a special type of bacteria inhabiting the mucous membrane of the stomach and duodenum of patients with peptic ulcer disease. In 2005, the authors of the article, Australian scientists Barry Marshall and Robin Warren, were awarded the Nobel Prize for the discovery of the bacterium Helicobacter pylori and its role in the pathogenesis of peptic ulcer disease. On this moment H. pylori infection is considered the main etiopathogenetic factor of peptic ulcer disease.
As it turned out, this type of bacteria is adapted to survive in conditions of low acidity existing in the stomach. With an increased release of hydrochloric acid in the stomach, H. pylori is able to colonize only the antrum and foci of gastric metaplasia of the epithelium in the duodenum; with low secretion of hydrochloric acid, the microbe can colonize any part of the gastric mucosa. The microbe reproduces mainly in the mucus-forming cells of the gastric mucosa. At the same time, the secretion of mucus by these cells is disrupted and, therefore, one of the important protective barriers of the mucous membrane is damaged (the mucus layer contains bicarbonates that neutralize hydrochloric acid). Also, a local inflammatory reaction (response to the penetration of H. pylori into the mucous membrane) stimulates the release of hydrochloric acid. It is possible that a certain role in the pathogenesis of peptic ulcer disease is played by the violation of microcirculation in the submucosa, as well as autoimmune reactions caused by H. pylori infection.
The possibility of Helicobacter pylori colonization of the duodenum is due to the formation of foci of gastric metaplasia of the intestinal epithelium. Foci of gastric metaplasia of the duodenal epithelium are areas of the mucous membrane of the small intestine, lined with gastric-type epithelium. The formation of such areas occurs mainly under the influence of pronounced acid aggression, in which the intestinal epithelium of the duodenum turns into the gastric epithelium, which is more resistant to acid. In areas of gastric metaplasia of the intestinal epithelium, H. pylori is able to multiply as well as the gastric mucosa. The mucus-secreting cells necessary for reproduction are also present in the foci of gastric metaplasia of the intestinal epithelium.
Damaging factors of H. pylori:
1. High penetrating ability - curved shape, presence of flagella, presence of phospholipase A and C, ability to adhere to epithelial cells;
2. Enzymatic activity - urease (hypergastrinemia, hyperchlorhydria), the formation of cytotoxic products (hydroxyamine, monochloramine); mucinase (reducing the viscosity of mucus), catalase - reducing the bactericidal effect of neutrophils;
3. Cytotoxicity - the appearance, possibly under the influence of antibiotics, cytotoxic strains, antibodies to Hp, cytokines, interleukins - mediators of inflammation.
Thus, the main etiopathogenetic factors of PUD can be identified:
Helicobacter pylori;
recurrent neuro-emotional stress;
eating disorder;
hereditary predisposition.
The clinical picture. Complaints are varied and are largely determined by the localization of the ulcer and the acidity of gastric juice. With ulcers of the posterior wall of the body of the stomach and cardia, pain occurs after eating, localized under the xiphoid process, here a positive Mendel's symptom is determined (pain of the anterior abdominal wall in the epigastric region during percussion). The pains are aching, dull, often radiating behind the sternum, into the region of the heart. Vomiting is relatively rare; nausea and heartburn prevail. Lesser curvature ulcers are characterized by pain in the epigastric region and rhythm: 15-60 minutes after eating. Antral ulcers are characterized by a clear periodicity and "hunger pains", a tendency to profuse bleeding; the secretory function of the stomach is increased.
The main symptom of duodenal ulcer is late pain (1.5-3 hours after eating), hungry, nighttime, subside after eating and antacids. Pain is localized in the epigastric region, sometimes near the navel and in the upper right quadrant of the abdomen, often radiating to the back, sometimes behind the sternum. The pains are often cutting, piercing, less often dull pains. Constant pain with a specific localization is characteristic of penetrating ulcers. The second most important symptom is vomiting, usually at the height of the exacerbation of the disease, which usually causes relief of pain. Of the dyspeptic disorders, heartburn is most often noted, sometimes as the only symptom of the disease. Sour belching is less characteristic, more often after eating. Appetite is usually not disturbed. There is a tendency to constipation. There is often a seasonal character of exacerbations (in spring and autumn). The tongue is usually coated with a white coating. Local or diffuse pain on palpation in the epigastric region with duodenal ulcer.
Combinations of gastric and duodenal ulcers are also possible. The pain syndrome in this case is characterized by two waves: after 40-60 minutes painful sensations appear, which sharply intensify after 1.5-2 hours and continue for a long time. Vomiting and persistent heartburn are observed.
Pain relieves spazgan, no-shpa, atropine and other antispasmodics, antacids (almagel, phosphalugel, rennie and others). A heating pad also helps, traces after it (pigmentation of the skin of the abdomen) may indicate peptic ulcer disease.
Dyspeptic phenomena:
1. Heartburn. Equivalent to pain. Immediately or 2-3 hours after eating, it is most typical for localization in the duodenal bulb, reflux esophagitis.
2. Belching, often with air. More common in stomach ulcers. Eating rotten may indicate pyloric stenosis.
3. Nausea - more common with antral ulcers.
4. Vomiting occurs at the height of pain and brings relief, a frequent symptom in functional or organic pyloric stenosis.
5. Appetite is usually preserved or increased, especially with duodenal ulcer, but steophobia occurs - fear of eating due to expected pain.
6. Constipation for 3-5 days, typical for the localization of ulcers in the bulb of the duodenum, "sheep" stool, which is caused by spastic dyskinesia of the large intestine.
With a long history of ulcers, atrophic processes develop in the gastric mucosa, acid production decreases, which is accompanied by a decrease in appetite, and a tendency to diarrhea appears.
Changes from the central nervous system - bad dream, irritability, emotional lability are often present with duodenal ulcer.
In thin, asthenic people, duodenal ulcer is more common. Weight loss may occur, although this is not always the case. Often, pronounced red dermographism, hyperhidrosis of the palms is detected.
Peptic ulcer disease is realized not without the participation of other organs and systems, for example, with a pyloroduodenal ulcer, anxiety, suspiciousness, egocentrism, increased claims, anxiety-phobic, hypochondriacal syndromes were noted.
Peculiarities of peptic ulcer disease in the elderly. If an ulcer is formed in patients over 40-50 years old, then an erased course is more often observed, there is no pain, dyspeptic disorders. Differential diagnostics with stomach cancer is carried out. In addition, in elderly patients, an ulcer can be combined with angina pectoris of abdominal localization, manifested during hard work, in such patients it is necessary to exclude atherosclerosis of the mesenteric vessels and the abdominal aorta.
Diagnostics.
Laboratory methods:
Blood test;
Fecal occult blood test;
Histological and cytological examination of gastrobiopsy specimens;
Determination of Нр in the gastric mucosa by two methods;
Total protein and protein fractions;
Analysis of urine.
A clinical analysis of blood can reveal hypochromic anemia with bleeding ulcers and erosions.
Feces for occult blood - Gregersen's reaction. Before the study, products containing iron are excluded 3 days in advance, you should refrain from brushing when brushing your teeth.
Methods for determining Нр in the gastric mucosa: serological - determination of the level of antibodies in the blood, morphological, microbiological and rapid urease test - examination of gastrobiopsy specimens, respiratory urease test, detection of AgHelicobacterrylori in feces using PCR and other methods.
Instrumental methods:
EGDS with targeted biopsy;
Ultrasound of the pancreas, liver, biliary tract;
pH - metry;
Rg - stomach graphy.
EGDS allows to reveal an ulcer defect, assess the state of the mucous membrane of the stomach and duodenum, assess the acid-forming function of the stomach and the contamination of Helicobacterрylori, and obtain gastro-biopsy specimens.
Study of the acid-forming function of the stomach - if necessary, intragastric pH-metry is performed - a diagnostic procedure during which acidity is measured directly in the gastrointestinal tract. Typically, intragastric pH metering refers to the measurement of acidity in the esophagus, stomach and duodenum.
Probeless and direct (probe) methods for the study of gastric juice are currently not used.
X-ray changes: "niche" - the availability of verification of an ulcer defect of at least 2 mm, convergence of folds, an annular inflammatory cushion around the niche, cicatricial deformities. Indirect signs - excessive peristalsis of the stomach, retraction along the greater curvature ("finger" symptom). Radiographically, duodenal ulcers are found more often when localized on the anterior and posterior walls of the bulb.
X-ray examination of the stomach is carried out for differential diagnosis with gastric cancer, in particular with primary ulcerative cancer.
X-ray examination is necessary in the diagnosis of pylorus stenosis. Determined by a high-beginning enhanced, gastric peristalsis, then marked expansion of the stomach with a significant amount of fasting contents, and weakening gastric peristalsis. The main symptom is a violation of the evacuation function of the stomach - the contrast agent remains in it for 6 or more hours.
Complications of peptic ulcer disease.Bleeding. In this case, vomiting occurs, the color of coffee grounds, but it can be without admixture of blood. Tarry stools (melena), often accompanied by hemodynamic disorders, acute post-hemorrhagic anemia may occur. Bleeding may be the first manifestation of peptic ulcer disease, which often occurs without pain. Treatment is conservative (hemostatic, replenishment of fluid and erythrocyte mass), endoscopic, and, if necessary, surgical.
Perforation characterized by the development of dagger pains, vomiting, a sharp deterioration in the condition. Symptoms of peritonitis develop. Perforation may occur subacutely if the gland covers the perforation. Emergency surgery is required. Clinical signs - positive peritoneal symptoms, hepatic dullness is not determined, laboratory - positive acute phase indicators, X-ray - the accumulation of gas in the subphrenic space is determined.
Periduodenitis, perigastritis, perivisceritis characterized by a change in the nature of the pain syndrome, the rhythm of pain disappears, the pain becomes constant, intense, especially during physical exertion, the nature of the irradiation changes.
Penetration ulcers most commonly occur in the pancreas. In this case, there is a sharp increase in pain, the cyclicality of the pain syndrome is lost. The pains are of a girdle nature, radiate to the back, and are aggravated by eating.
Malignancy- degeneration of an ulcer into cancer. A duodenal ulcer almost never degenerates into cancer.
Ulcers of the lesser curvature of the stomach, ulcers of the antrum and subcardial sections are malignant. Frequency disappears during the ulcerative process. The pain is mild, constant in nature, persists at night, does not depend on food intake. Loss of appetite, weight loss, general weakness. Anemia develops. There is latent blood in the stool. The general acidity of gastric juice remains, the amount of free hydrochloric acid decreases. X-ray reveals an increase in the size of the niche up to 2.5 cm and more, the erosion of its contours.
Most often, there is a primary ulcerative form of cancer. Elderly persons are prone to this. The pain is constant, the appetite disappears, there is an aversion to meat, a frequent complaint of nausea, vomiting that does not bring relief, and a decrease in body weight. Characterized by a decrease in gastric secretion up to achlorhydria, a persistent positive Gregersen reaction, increased ESR, anemization.
Gatekeeper stenosis- functional (eliminated by taking anticholinergics) and organic is observed in 1% of cases. Requires surgical treatment. The syndrome of high intestinal obstruction prevails, and not painful. Characterized by gastric dyspepsia (vomiting of food eaten, the frequency depends on the stage of stenosis, a constant feeling of heaviness in the epigastric region, stool retention, the appearance of vomit with a putrid odor in the later stages).
Treatment. The purpose of antiulcer treatment is to restore the mucous membrane of the stomach and duodenum (ulcer scarring) and maintain a long-term relapse-free course of the disease.
To achieve this goal, it is necessary to solve several problems:
to reduce the level of acid-peptic factor under the condition of intensive acid production in the stomach according to the data of a pH-metric study;
restore the motility of the gastroduodenal zone;
to carry out eradication therapy Helicobacter rulori, the presence of which has been proven by two research methods;
determine the individual volume of therapy after anti-Helicobacter pylori therapy (the period of treatment until the ulcer defect heals and control gastroduodenoscopy);
increase the resistance of the mucous membrane of the gastroduodenal zone;
carry out psycho-emotional correction of the patient;
to include in complex therapy means taking into account concomitant diseases;
to outline the ways of preventive therapy for exacerbation of peptic ulcer disease.
Diet is not a critical factor. Modern treatment regimens can significantly expand the diet of most patients with peptic ulcer disease. Strict chemical and mechanical sparing is necessary only during the period of severe pain syndrome Table - 1, 1-A, 1-B. The main principle of the diet is to reduce the portion and increase the frequency of food intake (preferably at least 6 times a day), since food has antacid and buffer properties, especially protein foods. Complete protein nutrition - up to 140g of proteins per day, accelerates the regeneration of the mucous membrane of the stomach and duodenum.
Bed rest is not required. Most patients are treated on an outpatient basis.
The success of the treatment of peptic ulcer disease is determined primarily by the mandatory implementation by the patient of general recommendations, which include the following:
exclusion of taking ulcerogenic drugs;
prevention or elimination of stressful circumstances;
smoking cessation and alcohol abuse.
Medication.
Peptic ulcer therapy principles:
Suppression of aggressive factors;
Stimulation of defense factors;
Helicobacter pylori therapy.
The main groups of antiulcer drugs:
1. Drugs that inhibit the secretion of HCl:
Proton pump blockers;
H 2 blockers;
M-anticholinergics;
Prostanglandins.
2.Preparations neutralizing HCl:
Absorbable antacids;
Non-absorbable antacids.
3.Preparations that form a protective film over the ulcer:
Sucralfate;
4. Drugs stimulating defense factors:
Prostaglandins;
Carbenoxolone;
First-line anti-Helicobacter pylori therapy.
Proton pump blockers:
Omeprazole (Omez) 20 mg 2 times a day, or
Lanzoprazole (Lanzap) 30 mg 2 times a day, or
Pantoprazole 40mg 2 times a day, or
Rabeprazole (Pariet) 20 mg 2 times a day, or
Esomeprazole (Nexium) 40 mg daily.
Antibiotics:
Clarithromycin 500 mg 2 times a day, or
Amoxicillin 1000 mg 2 times a day, or
Metronidazole 500 mg 2 times a day.
Second-line anti-helicobacter therapy.
Duration of treatment: 10 - 14 days.
Proton pump blockers;
Preparations of bismuth salts (de-nol 120 mg 4 times a day);
Antibiotics:
tetracycline 500 mg 4 times a day and
metronidazole 500 mg 3 times a day
Rules for the use of anti-Helicobacter pylori therapy:
If the use of the treatment regimen does not lead to the onset of eradication, it should not be repeated;
If the scheme used did not lead to eradication, this means that the bacterium has acquired resistance to one of the components of the treatment regimen (nitroimidazole derivatives, macrolides);
If the use of one and then the other treatment regimens does not lead to the onset of eradication, then the sensitivity of the H. pylori strain to the entire spectrum of antibiotics used should be determined;
The appearance of bacteria in the patient's body a year after treatment should be regarded as a relapse of the infection, and not reinfection. In case of recurrence of infection, it is necessary to use more effective treatment regimens.
None of the above treatment regimens led to 100% eradication over the long period of study.
Perspectives in the treatment of Helicobacter pylori infection:
Medicinal blockade of Helicobacter pylori urease;
The use of drugs that prevent the adhesion of Helicobacter pylori (rebamipide, ekabet);
Creation of a vaccine against Helicobacter pylori infection.
Under peptic ulcer means a chronic recurrent disease characterized by a common morphological feature - the loss of mucosal areas in those areas of the digestive tract that are in contact with active gastric juice (stomach, proximal part of the duodenum).
Along with peptic ulcer disease as an independent nosological form, it is now accepted to distinguish secondary, symptomatic ulcers and gastroduodenal ulcers arising under the influence of a known etiological factor - stress, disorders of local and regional blood circulation, intake of non-steroidal anti-inflammatory drugs, etc. save for stomach and duodenal ulcers, the origin of which remains unknown.
I'm a peptic ulcer widespread in all countries of the world. Among patients who were hospitalized with diseases of the digestive system, peptic ulcer disease is diagnosed in 35.8% of cases. In countries Western Europe, SSA and Japan, up to 2-3% of the adult population suffer from peptic ulcer disease. However, these figures do not give a complete picture of the true incidence of the disease, since they are mainly based on the number of patients seeking medical help.
The ratio of stomach and duodenal ulcers largely depends on the age of the patients and the region of residence. In persons young age duodenal ulcers prevail - 16: 1 (over the age of 60 years - 2: 1). The ratio of stomach ulcers and duodenal ulcers on average in Europe and SSA is 1: 4, in India - 1:19 and even 1:32. In Japan, on the contrary, gastric localization of ulcers prevails (2: 1), and in people living in the highlands of the Andes, this figure is even higher (20: 1).
On the basis of epidemic studies, a number of factors are identified that contribute to the more frequent disease of peptic ulcer disease.
It is generally accepted that men get sick more often than women. However, the ratio of men and women suffering from peptic ulcer disease varies depending on the age of the patients. So, men at a young age suffer from peptic ulcer disease 3-5 times more often than women, and at the age of over 50 years (after the onset of menopause in women) this difference is leveled. In recent decades, there has been a noticeable increase in the incidence of peptic ulcer disease in women, which is due to stressful situations, the increasing prevalence of bad habits (smoking, alcohol) among women, more frequent use of analgesic drugs, as well as disorders of the hormonal function of the ovaries.
Peptic ulcer disease among the urban population is recorded more often than among the rural. High level morbidity due to dietary habits, social and industrial life, pollution external environment in cities.
The so-called acute professions are distinguished: pilots, machinists, operators, dispatchers, conveyor workers, etc. Almost any work, if it is associated with psycho-emotional overload, physical stress, frequent business trips, lack of adequate rest, is a significant factor predisposing to ulcerative disease. disease.
During periods of major social upheavals, accompanied by a sharp deterioration in nutrition, material living conditions of the population as a whole, and mental trauma, there is an increase in peptic ulcer disease and its complications.
It was found that persons with a burdened heredity, other things being equal, are much more likely to suffer from peptic ulcer disease, especially in childhood, adolescence and young age.
Risk factors also include bad habits and dietary habits (smoking, drinking strong alcoholic beverages, alimentary inaccuracies, violation of the rhythm of food intake).
Over the past 10-15 years, in many countries of the world, including ours, there has been a tendency towards a decrease in the incidence of peptic ulcer disease, as well as the number of hospitalizations, the frequency of surgical interventions and deaths with this disease.
At the same time, a number of researchers note an increase in the incidence of peptic ulcer disease. The observed increase in the incidence of peptic ulcer disease, apparently, is explained not by a true increase in the incidence, but by an improvement in the quality of diagnosis.
What provokes peptic ulcer
Currently, it is generally accepted that peptic ulcer disease is a polyetiological disease. All known etiological factors can be divided into two main groups: predisposing, contributing to the development of the disease and realizing the onset or recurrence of peptic ulcer disease.
Hereditary constitutional factors. Among the etiological factors leading to the development of peptic ulcer disease, the most important place is occupied by a hereditary predisposition. The frequency of hereditary burden, according to the literature, in patients with peptic ulcer disease is 5.5-50%. Discrepancies in assessing the role of heredity in the occurrence of peptic ulcer disease are associated with different approach to conduct the research. Only with the purposeful collection of a family history with the maximum coverage of relatives, with widespread use in their examination, along with the X-ray endoscopic method, can one get a true idea of the effect hereditary factors on the development of the disease. Thus, during a special genetic examination, it was noted that the prevalence of peptic ulcer disease in the relatives of the probands was 5-10 times higher than in the relatives. healthy people.
Another proof of the importance of hereditary burdening can be the concordance of occurrence and identity of the localization of peptic ulcer disease in monozygous twins.
Currently, a number of specific genetic factors have been identified that determine a hereditary predisposition to peptic ulcer disease.
Evidence-based genetic factors include indicators of the maximum secretion of hydrochloric acid, the content of pepsinogen-I in the blood serum, and an increase in the release of gastrin in response to food. Among the factors, presumably having a hereditary basis, the authors include the content of pepsinogen-II in the blood serum; some deviations in the processes of secretion of hydrochloric acid (an increase in its release after eating, an increase in the sensitivity of the parietal cells to gastrin, a violation of the mechanism feedback between the production of hydrochloric acid and the release of gastrin); disorders of the motor function of the stomach and duodenum (rapid gastric emptying, duodenogastric reflux); a decrease in the activity of the enzyme a-antitrypsin; the content of adrenaline in plasma and acetylcholinesterase in blood serum and erythrocytes; violation of the production of immunoglobulin A; the nature of salivation in response to citric acid; morphological changes in the mucous membrane (gastritis, duodenitis).
Among the genetically determined factors of peptic ulcer disease, an important place is given to the group specificity of blood, its Rh-relevance, the ability to secrete antigens of the AVN system, the identification of the HLA-antigen of histocompatibility B5, B15, B35.
In addition, other genetic markers of susceptibility to peptic ulcer disease are distinguished: the absence of an intestinal component and a decrease in the B index of alkaline phosphatase, the absence of the 3rd fraction of cholinesterase, the ability to sense the taste of phenylthiocarbamide.
It should also be borne in mind that a certain type of higher nervous activity, personality traits, anthropological features predisposing to the development of the disease. So, among patients with peptic ulcer, there is a predominance of persons with inert inhibitory and excitatory processes, as well as a weak type of higher nervous activity. When studying the psychoemotional status using a personality test, they show a significant increase in indicators on the scales of anxiety, egocentrism, claims, demonstrativeness. It was noticed among those suffering from this disease the predominance of people of asthenic physique, however, at present, the type of physique is not given much importance in the etiology of peptic ulcer disease.
For a long time, when explaining the genetics of peptic ulcer, a polygenic hypothesis was used, according to which the hereditary component of this disease is due to a number of genes acting together (polygenic). Clinically, the disease develops when the number of certain genes exceeds a threshold level. The polygenic hypothesis assumes that all ulcers are a type of one disease. An alternative to the polygenic concept is the hypothesis of the heterogeneity of the disease, according to which there are many forms of peptic ulcer.
Genetic differences between "childhood" and "adult" ulcers, mediogastric and pyloroduodenal ulcers are a significant confirmation of the heterogeneity of the disease.
Hereditary burden is the most important etiological factor of peptic ulcer disease. However, it creates only a predisposition to the disease, which is realized only in combination with other adverse effects (neuropsychic overload, alimentary errors, bad habits, taking "ulcerogenic" drugs, etc.).
Neuropsychic factors... The influence of neuropsychic factors on the occurrence of peptic ulcer disease is assessed ambiguously. However, most scientists assign them a significant role in the etiology of the disease. In ulcerogenesis, the main role is played by a functional disorder of the autonomic nervous system with a predominance of the tone of the vagus nerve. Hypervagotonia causes a spasm of the muscles and blood vessels, resulting in ischemia, a decrease in tissue resistance and subsequent digestion of the mucous membrane by gastric juice.
The recognition of the decisive role of neuropsychic factors in the etiology of peptic ulcer disease was reflected in the cortico-visceral theory. According to the cortico-visceral theory, the triggering mechanism of ulcerogenesis is shifts in higher nervous activity arising from negative emotions, mental overstrain, etc. At the same time, a weakening of the inhibitory process in the cerebral cortex and excitation (disinhibition) of the subcortex, in which a focus of stagnant excitement, which is accompanied by an increase in the tone of the vagus and sympathetic nerves. Dysfunction of the autonomic nervous system leads to an increase in gastric secretion, increased motility, spastic vascular contractions and trophic changes in the mucous membrane of the gastroduodenal zone, and ultimately to ulceration. It should be noted that the cortico-visceral theory of the development of peptic ulcer did not take into account the complex biochemical mechanisms, the hormonal link of regulation, differed in schematism and was not always based on facts. Therefore, in its original form, it has few supporters. At the same time, some of the provisions of this theory have found further development in modern experimental and clinical research.
Many scientists attach great importance to stressful situations, considering peptic ulcer disease as special case maladjustment, as a breakdown of compensatory-adaptive mechanisms with excessive force of adverse factors.
Currently, the development of some diseases, in particular peptic ulcer disease, is considered from the standpoint of violation biological rhythm various physiological processes of the human body. An illustrative example disturbances in the biological rhythm in patients with peptic ulcer disease is nocturnal gastric hypersecretion, which often precedes the development of gastroduodenal ulcers.
Thus, neuropsychic overload, disorders of psychophysiological functions can be realizing factors in the onset of peptic ulcer disease.
Alimentary factor. Currently, there is a tendency to revise the influence of violations of the regime and the nature of nutrition on the development of peptic ulcer disease. According to foreign researchers, there is no direct evidence of the influence of food on the occurrence of gastroduodenal ulcers.
However, everyday experience teaches that in many patients the onset and relapses of peptic ulcer disease occur after errors in food or a disturbance in the rhythm of food intake. Symptoms such as heartburn, sour belching, and vomiting often occur after eating irritating and saponified food. Convincing clinical and experimental data proving the role of the nutritional factor were obtained when studying the dietary habits of the Indian population in regions with high and low incidence of peptic ulcer disease.
The harmful effects of food on the mucous membrane of the gastrointestinal tract can be different. Some food components stimulate gastric secretion with low buffering properties. Long-term use of rough food contributes to the development of chronic gastritis and gastroduodenitis, considered as pre-ulcer conditions. In turn, the buffering and antacid properties of some products (meat, milk, etc.) have a clear anticorrosive effect, blocking active gastric juice.
Bad habits. TO bad habits, contributing to the development of peptic ulcer disease, primarily include smoking and alcohol abuse.
Among smoking men, peptic ulcer disease occurs 2 times more often than among nonsmokers. Nicotine causes vasoconstriction in the stomach, somewhat enhances its secretion, increases the concentration of pepsinogen-1, leads to accelerated evacuation of food from the stomach, reduces pressure in the pyloric sphincter and promotes duodenogastric reflux. In addition, nicotine inhibits the secretion of bicarbonates of the pancreas, disrupts mucus production and reduces the synthesis of prostaglandins in the mucous membrane.
Alcohol in the etiology of peptic ulcer disease plays a multifaceted role. Firstly, it stimulates the acid-forming activity of the stomach, as a result of which the aggressive properties of gastric juice are enhanced. Secondly, it disrupts the barrier function of the mucous membrane. Thirdly, with prolonged use of spirits, chronic gastritis and duodenitis develop, and the resistance of the mucous membrane decreases. Clinical experience testifies that peptic ulcer disease and its relapses are often provoked by alcoholic excesses in combination with gross errors in food.
Excessive consumption of coffee can also be attributed to bad habits. The mechanism of the adverse effect of coffee is associated with the stimulating effect of caffeine on the acid-forming function of the stomach.
Medicinal effects. Clinically and experimentally, it has been proven that a number of drugs (non-steroidal anti-inflammatory drugs, corticosteroids, reserpine, etc.) can cause ulceration of the mucous membrane of the stomach or duodenum.
The ulcerogenic effect of these drugs is realized in various ways. Non-steroidal anti-inflammatory drugs, primarily acetylsalicylic acid, reduce mucus production, change its qualitative composition, suppress the synthesis of endogenous prostaglandins and disrupt the protective properties of the mucous membrane; their direct effect on the gastric mucosa with the formation of acute ulcers and erosions is not excluded. Other drugs (reserpine, corticosteroid drugs) predominantly enhance the aggressive properties of gastric juice, directly stimulating the production of hydrochloric acid by the parietal cells or acting through the neuroendocrine apparatus.
Helicobacter pylori. In 1984, Australian researchers B. Marshall and J. Warren discovered a new bacterium, which they called Campylobacter pylori, which was isolated from the gastric mucosa of patients suffering from chronic gastritis. Later Campylobacter pylori was renamed Helicobacter pylori (HP). HP is predominantly found in the antrum of the stomach under a layer of mucus on the surface of epithelial cells. In the duodenum, HP is found only in areas of gastric metaplasia. It has been shown that HP damages the gastric mucosa and is an etiological factor in the development of active antral gastritis (type B). In this form of gastritis, HP is found in almost 100% of cases, while on the unchanged mucous membrane of the antral part of the stomach - only in 8-10%.
The role of HP in the etiology of peptic ulcer disease remains controversial. In favor of the fact that HP is directly related to peptic ulcer disease, the following arguments are put forward:
- frequent detection of HP in peptic ulcer disease (up to 75% for stomach ulcers and 95% for duodenal ulcers);
- healing of ulcers after treatment with antibiotics and bismuth subcitrate, which destroy HP;
- connection of recurrence of gastroduodenal ulcers with preservation of HP.
Against this assumption is evidenced by the fact that under experimental conditions it is possible to reproduce Helicobacter pylori gastritis, but not an ulcer. Peptic ulcer disease has no epidemiological characteristics of infection. Spontaneous healing of the ulcer does not occur with the disappearance of HP. With age, the frequency of Helicobacter pylori gastritis increases, and duodenal ulcers decreases. It is also unclear why the ulcer is localized more often in the duodenum, and not in the stomach, where HP colonization is always more pronounced. Thus, the whole problem of the etiology of peptic ulcer disease cannot be reduced only to HP infection. Apparently, the active antral gastritis caused by HP contributes to the development of peptic ulcer disease in persons genetically predisposed to this disease.
Diseases contributing to the development of peptic ulcer. Along with the above etiological factors, there is evidence that peptic ulcer disease occurs much more often in a number of diseases internal organs... These diseases primarily include chronic diseases lungs, cardiovascular system, liver, pancreas, accompanied by functional insufficiency of these organs and systems.
Thus, peptic ulcer disease is a polyetiological disease. For its occurrence, it is necessary to influence not an isolated causal factor, but the sum of factors in their interaction. In this case, hereditary burden should be considered as a predisposing background against which the action of other, usually several, etiological factors is realized.
The role of etiological factors is different depending on the age, sex of the patient and the location of the ulcer. So, at a young age, heredity is of greatest importance. In middle age, among the causes of the disease, neuropsychic overstrain, bad habits, and gross errors in nutrition begin to prevail. In old age, in the genesis of peptic ulcer disease, a significant specific gravity acquire "ulcerogenic" drugs, various concomitant diseases.
Pathogenesis (what happens?) During peptic ulcer disease
Ideas about the pathogenesis of peptic ulcer disease changed depending on the prevailing views at certain periods. In most of the assumed theories of pathogenesis, the cause of ulceration was tried to be explained from some one point of view: inflammation, mechanical damage, vascular disorders, acid-peptic effect, impaired mucus formation, reverse diffusion of H +, duodenogastric reflux of bile, etc.
Numerous clinical and experimental studies in recent years have significantly expanded our understanding of the local and neurohumoral mechanisms of ulcerogenesis. WITH modern point vision, the pathogenesis of peptic ulcer disease appears to be the result of an imbalance between the factors of aggression of gastric juice and the protection of the mucous membrane of the stomach and duodenum.
Aggressive factors include hydrochloric acid, pepsin, impaired gastric evacuation and duodenogastric reflux.
Acid-peptic factor. Highest value in the mechanisms of formation of gastroduodenal ulcers is given to the acid-peptic factor. As evidence of the role of hydrochloric acid in ulcerogenesis, the following data are carried out: the practical absence of cases of gastroduodenal ulcers with reliably established achlorhydria; the occurrence of ulcers only in areas of the digestive tract in contact with active gastric juice; good therapeutic effect of antacids and drugs that block the release of hydrochloric acid; recurrence of ulcers after surgery only while maintaining gastric acid secretion. This position is confirmed by a "natural experiment" - the Zollinger-Ellison syndrome.
Another component of the acid-peptic factor, in addition to hydrochloric acid, is a proteolytic enzyme - pepsin. The significance of the proteolytic activity of pensin in the genesis of ulcer formation is assessed ambiguously. According to a number of authors, ulceration is associated with peptic digestion, and hydrochloric acid is assigned the role of a regulator of enzymatic activity.
However, the opinion remains uncontested according to which pepsin, although it belongs to the indispensable factors of ulceration, in itself is not endowed with corrosiveness.
Disorders of gastroduodenal motility. In the mechanism of ulceration, in addition to the aggressiveness of the environment, the duration of contact of acidic gastric contents with the mucous membrane of one or another part of the gastroduodenal region plays a significant role. If there is a prolonged retention of the contents in the stomach, conditions are created for the development of gastric ulcers, on the contrary, with an intense intake of acidic contents from the stomach into the duodenum or a delay in evacuation along it due to duodenostasis, ulcers are formed in this department.
Duodenogastric reflux, resulting from the discoordination of the motor function of the duodenum and stomach against the background of the weakness of the pylorus, is given a certain importance in the mechanisms of development of stomach ulcers. With duodenogastric reflux, bile acids and lysolecithin enter the stomach. Under their influence, the barrier function of the mucous membrane is disrupted, the reverse diffusion of hydrogen ions is enhanced, which leads to local tissue acidosis and tissue necrosis with the formation of an ulcer.
The resistance of the mucous membrane of the stomach and duodenum to the damaging effect of hydrochloric acid, pepsin and bile acids depends on a complex of interrelated protective factors: the usefulness of the mucous barrier, sufficient blood supply to the mucous membrane and some other factors.
Protective barrier of the mucous membrane. It is customary to distinguish two components of the protective mucous barrier: a layer of visible, insoluble mucus ("first line of defense") and a layer of epithelial cells of the mucous membrane ("second line of defense").
Visible mucus (mucin) covers the entire mucous membrane of the stomach and duodenum with a thin layer of 1-1.5 mm. Mucus is tightly bound to the surface epithelium by colloidal strands. The composition of mucus is determined by two groups of substances: mucopolysaccharides and glycoproteins, which form complex high molecular weight structures that form a gel. The viscosity and ability of visible mucus to resist the digestive properties of gastric juice is provided with the participation of fucoglycoproteins and N-acetylneuraminic acid, which belongs to the group of sialomucins.
With a peptic ulcer, the total production of mucus may decrease or its qualitative composition may change. The reason for the development of peptic ulcer disease is genetically determined features of fucoglycoproteins, which impede their secretion.
The next anatomical substrate of the protective barrier is the cells of the superficial epithelium of the mucous membrane. The importance in the barrier function of the mucous membrane is the apical membrane of cells. The stability of the mucous membrane of the stomach and duodenum largely depends on its integrity and continuous renewal.
Active regeneration of the surface epithelium is considered as one of the important elements providing a sufficiently high resistance of the mucous membrane, and if it is damaged, the defect heals quickly. Chronic gastritis, which is based on diiregenerative shifts, in this regard, may contribute to the development of peptic ulcer disease.
Peptic ulcer-associated gastritis, is primarily Helicobacter pylori gastritis. The formation of gastric ulcers is associated with the fact that HP can secrete protease and cytotoxins, damage the surface epithelium and, by destroying the mucous barrier, create conditions for proteolysis of the stomach wall. The involvement of HP in the development of duodenal ulcers remains unclear. Scientists propose the following "pathogenetic cascade" initiated by H. pylori gastritis. Active inflammation of the antrum leads to an increase in the motor function of the stomach and the discharge of acidic gastric contents into the duodenum. Overproduction of HC1 is associated with the urease activity of HP. Urease breaks down urea to form ammonia, ammonia stimulates G-cells that produce gastrin, which in turn leads to HC1 hypersecretion. "Acidification" of the duodenum is accompanied by the appearance of islets of gastric metaplasia in it. In the islets of metaplasia, HP can colonize, active inflammation develops, as in the stomach; in the duodenum, these areas are rapidly destroyed and ulcers are formed.
In the mucous membrane of the gastroduodenal zone, physical and biochemical processes constantly occur, which prevent the reverse diffusion of hydrogen ions. Normal secretion of bicarbonates and mucus allows maintaining the pH on the surface of epithelial cells at 7.1-7.4 at a parietal pH of 1.4-2.0. A decrease in the secretion of bicarbonate by the gastric mucosa may play an important role in the formation of gastric ulcers.
In the pathogenesis of duodenal ulcer, one should take into account the possibility of reducing the production of pancreatic bicarbonates and "acidification" of the duodenal contents.
The role of vascular factor. As evidence of the important role of the vascular component in the development of gastroduodenal ulcers, the following facts are given:
- changes in blood vessels in the ulcer zone (sclerotic lesions of terminal arterioles and their obliteration, dilatation of veins and capillaries, microcirculation disorder);
- the incidence of peptic ulcer disease in persons with severe stenosis of the celiac trunk and with specific changes in the vessels of the submucosal layer, characteristic of hypertension and diabetes mellitus, is many times higher than the standardized indicators of the incidence of peptic ulcer disease;
- the results of experimental studies showing that ischemia has a significant effect on the state of the protective mucous barrier;
- good effect of hyperbaric oxygenation in the treatment of peptic ulcer disease.
Although the leading role of vascular lesions as one of the links in the pathogenesis of peptic ulcer disease is not in doubt, this factor acquires an independent significance only in some types of symptomatic gastroduodenal ulcers. So, microcirculation disorders in the mucous membrane are the main pathogenetic link of stress ulcers, lesions of regional arteries - "senile" ulcers, specific changes in the vessels of the submucosal layer - ulcers in hypertension.
Currently, the role of prostaglandins and immune disorders in the pathogenesis of peptic ulcer disease is being actively studied.
Prostaglandins. Prostaglandins are biologically active substances and are derived from fatty acids. Clinical and experimental observations have shown that prostaglandins have an antiulcer effect and can prevent the development of gastroduodenal ulceration when exposed to alcohol, salicylates, indomethacin, glucocorticoid drugs.
The mechanism of the protective action of prostaglandins is not fully understood. It is believed that prostaglandins provide reliable stability of the gastroduodenal mucosa due to their ability to inhibit the production of hydrochloric acid, stimulate mucus formation and the production of an alkaline component of gastric juice, and increase the level of blood flow in the mucous membrane and its regenerative potency. However, the role of prostaglandins in ulcerogenesis needs further study, since it has been noted that their concentration in the blood serum and in the gastroduodenal mucosa in healthy people and patients with peptic ulcer disease may practically not differ.
Immune factors. Recent studies have shown that a variety of immune shifts are observed in peptic ulcer disease.
The balance between the factors of aggression of gastric juice and protection of the mucous membrane of the stomach and duodenum in different phases of digestion under changing conditions of external and internal environment the organism is supported by the coordinated interaction of the neuroendocrine system. Violations of the integration and coordination functions of this system can play an important role in the pathogenesis of peptic ulcer disease.
Neuroendocrine factors of pathogenesis. The neuroendocrine system, which regulates various functions of the digestive organs, includes the parasympathetic link of the autonomic nervous system; sympathetic-adrenal system; system hypothalamus - pituitary gland - peripheral endocrine glands and gastrointestinal hormones. The central place in this system belongs to the hypothalamic region. The cerebral cortex realizes its influence through the hypothalamus, which, however, does not mean constant interference of the cortex in its function; cortical influence is included only in "extreme", extreme situations... Under normal conditions, the hypothalamus constantly monitors and corrects the activity of the endocrine glands and the autonomic nervous system. It has now been established that there are perfected self-regulation of tissue and cellular levels (protein synthesis by the cell, transport of electrolytes and water, cell energetics, etc.), closed self-regulation systems, for example, gastroduodenal, afferent connections of these systems with the higher parts of the central nervous system with the presence of feedbacks.
The discovery of gastrointestinal hormones - peptides that regulate various functions of the gastrointestinal tract - is rightfully considered one of the greatest achievements in biology in recent years. Their total number is enormous, the mass significantly exceeds the mass of any endocrine gland. Endocrine cells are localized mainly around the nerve endings and vessels of the mucous membrane, which suggests a neuroendocrine complex. The close relationship and mutual influence of the nervous and hormonal regulatory systems is indicated by the detection of certain peptide hormones of the gastrointestinal tract (gastrin, bombesin, vasoactive intestinal polypeptide) in the structures of the brain, and, conversely, hormones first discovered in brain cells (somatostatin, neurotensin, substance P, enkephalins), as well as "pituitary" hormones are found in endocrine cells and nerve fibers of the gastrointestinal tract.
Gastrointestinal hormones have a wide spectrum of action on various functions of the stomach and duodenum, violations of which can be of no small importance in the pathogenesis of peptic ulcer disease. Polypeptide hormones stimulate (gastrin, bombesin) or inhibit (somatostatin, vasoactive intestinal peptide, gastric anhibitor peptide) the production of hydrochloric acid, excite (secretin, substance P) or suppress (somatostatin, neurotensin) the active secretion of pancreatic bicarbonate tract (motilin), increase the production of gastric mucus (somatostatin, bombesin), increase blood flow and regenerative processes in the gastric mucosa (gastrin).
Assessment of the role of neuroendocrine disorders in the pathogenesis of peptic ulcer disease is controversial. For the occurrence of peptic ulcer disease, it is necessary to summarize a number of etiological factors and include in a certain sequence a complex and multicomponent system of pathogenetic links, which ultimately leads to the formation of ulcers in the gastroduodenal zone
The morphological substrate of peptic ulcer disease is a chronic ulcer of the stomach or duodenum. Stomach ulcer in 85% of cases is single, in 15% - multiple. Duodenal ulcer is usually solitary. In 3% of cases, there is a combination of stomach ulcers and duodenal ulcers.
A stomach ulcer is usually located on the lesser curvature in the prepyloric and pyloric regions, much more rarely in the cardiac and subcardial regions; usually it is found on the border of the zones of the gastric and pyloric glands proper, where during the movements of the stomach the greatest stretching of its muscular membrane is noted. Duodenal ulcer is localized more often in its upper (bulbar) part, less often in other parts of the intestine (extrabulbar ulcers). Usually it is located in the area of transition of the mucous membrane of the duodenum into the mucous membrane of the stomach, that is, in the area that is also subjected to stretching during the peristaltic movements of the intestine.
The ulcer has an oval or round shape (ulcus rotundum) and sizes from several millimeters to 5-6 cm. It penetrates the stomach wall to different depths, sometimes reaching the serous layer. The bottom of the ulcer is smooth, sometimes rough, the edges are roller-shaped raised, dense callous (callous ulcer, from Latin callus - corn). The edge of the ulcer, facing the esophagus, is somewhat undermined, and the mucous membrane hangs over the defect, and the edge facing the gatekeeper is flat, looks like a terrace, the steps of which are formed by the layers of the wall - the mucous membrane, submucosa and muscle. This kind of edges is explained by the displacement of the layers during the peristalsis of the stomach, going from the esophagus to the pylorus. In cross section, a chronic ulcer has the shape of a truncated pyramid, the narrow end of which faces the esophagus. The serous membrane in the area of the ulcer is thickened, often soldered to the adjacent organs - the liver, pancreas, omentum, transverse colon.
The microscopic picture of chronic gastric ulcer in different periods of the course of peptic ulcer disease is different. During the period of exacerbation of peptic ulcer disease, a wide zone of fibrinoid necrosis appears in the area of the bottom and edges. Fibrinous-purulent or purulent exudate is located on the surface of the necrotic masses. The zone of necrosis is delimited by granulation tissue with a large number thin-walled vessels and cells, among which there are many eosinophils. Deeper behind the granulation tissue is coarse fibrous scar tissue. An exacerbation of an ulcer is indicated not only by exudative-necrotic changes in its bottom, but also by fibrinoid changes and inflammatory infiltration of the vessel walls, often with blood clots in their lumens, as well as mucoid and fibrinoid swelling of scar tissue at the bottom of the ulcer. In the intramural nerve plexuses, ganglion cells undergo hydropic degeneration, their nuclei become pyknotic; the plexuses themselves are infiltrated by lymphocytes and histiocytes. Growth of nerve fibers in the area of the ulcer is found. In its edges, hyperplasia and dysplasia of the proliferating epithelium are noted. In connection with these changes, the size of the ulcer increases, it becomes possible to destroy the entire wall of the stomach, which can lead to serious complications.
In cases where the exacerbation is replaced by remission (ulcer healing), inflammatory changes subside, necrotic masses are rejected and granulation tissue appears in their place, which matures into coarse-fibrous. The surface of the ulcer is covered with a regenerating flattened epithelium, which eventually becomes higher and begins to secrete mucus; gastric pits and glands are formed, which, in comparison with a normal stomach, have a simpler structure. Regeneration of the muscular plate of the mucous membrane is also possible, however, the elastic skeleton does not recover.The muscular membrane in the ulcer area is replaced by fibrous tissue. obliteration of vascular light As you can see, cicatricial changes ("scar after an ulcer") undergo the submucosa and the muscular membrane, and not the gastric mucosa After healing of duodenal ulcers, scars may not form
Thus, an exacerbation of peptic ulcer disease, even in cases of a favorable outcome, leads to an increase in cicatricial changes in the stomach and aggravates the violation of the trophism of its tissues, including newly formed scar tissue, which is easily destroyed during the next exacerbation of peptic ulcer disease.
During remission of peptic ulcer disease, based on the characteristics of ulcer healing, scar tissue is found at the edges, the mucous membrane at the edges is thickened, hyperplastic In the bottom area, destroyed muscle layers and scar tissue covering it are visible, and the bottom of the ulcer is covered with a layer of epithelium Here, in the scar tissue , many vessels (arteries, veins) with thickened walls. In many vessels, the lumens are narrowed or obliterated due to the proliferation of intimal cells (endovasculitis) or the proliferation of connective tissue. Sometimes, in the bottom of the ulcer, among the scar tissue, there is a proliferation of nerve fibers like amputation neuromas.
The pathological anatomy of a chronic duodenal ulcer does not fundamentally differ from that of a chronic gastric ulcer.
Characteristic changes in peptic ulcer disease are also observed in areas remote from the ulcer. In case of peptic ulcer with localization of an ulcer in the stomach in the antrum and in the region of the edges of the ulcer, compared with the norm, the lymphoid-cell infiltration of the lamina propria increases, and the number of cells secreting mainly IgG increases. The accumulation of the same cells is detected in the connective tissue of the bottom of the ulcers.
These data indicate activity immune system with gastric ulcer, which is due to the antigenic properties of the decay products of the bottom of the ulcer, viruses and microorganisms, as well as the formation of autoantibodies. With duodenal ulcers, the gastric mucosa contains hyperplastic gastric glands proper, an increase in the number of major granulocytes is noted, as well as an almost twofold increase in the number of parietal granulocytes compared to the norm. With the help of electron microscopic examination, it was found that, along with hyperplasia of the glands, their accelerated differentiation occurs, due to which the number of mature functionally active cells that produce hydrochloric acid increases. In patients with duodenal ulcer, hyperplasia of cells producing gastrin is also noted, the number of which is almost twice as large as their number in gastric ulcers.
In the area of the gastric glands proper (in the area of the fundus of the stomach), changes in the type of chronic gastritis prevail; in the distal parts of the stomach, signs of atrophic gastritis with symptoms of intestinal metaplasia are often revealed.
With peptic ulcer disease, a variety of complications appear.
- ulcerative-destructive (bleeding, perforation, penetration);
- inflammatory (gastritis, duodenitis, perigastritis, periduodenitis);
- ulcerative cicatricial (narrowing of the inlet and outlet sections of the stomach, deformation of the stomach, narrowing of the lumen of the duodenum, deformation of its bulb);
- malignancy of the ulcer (the development of cancer from the ulcer);
- combined complications.
Bleeding is one of the most frequent and dangerous complications of peptic ulcer disease. There is no relationship between the incidence of bleeding and the localization of the ulcer in the stomach; when the ulcer is localized in the duodenum, bleeding is more often caused by ulcers located in the back wall of the bulb. Bleeding occurs due to erosion of the walls of blood vessels (arrosive bleeding), so it usually occurs during an exacerbation of peptic ulcer disease. Blood often remains in the stomach or intestines, partially excreted in vomit and feces. Vomit resembles coffee grounds due to changes in blood pigment under the influence of gastric juice. The feces become tarry.
Perforation (perforation) is also usually observed during an exacerbation of peptic ulcer disease. More often, pyloric stomach ulcers or ulcers of the anterior wall of the duodenal bulb are perforated. Perforation of the ulcer leads to peritonitis. Initially, inflammation in the form of fibrinous overlays on the peritoneum appears only in the area of the perforated opening, then it becomes widespread and not fibrinous, but fibrinous-purulent. In the presence of adhesions, perforation may be accompanied by only limited peritonitis. Chronic peritonitis is rare. Then the masses of gastric contents are encapsulated, granulomas are formed on the peritoneum and in the omentum. foreign bodies... V rare cases when the perforation is covered by the liver, omentum, pancreas or rapidly appearing fibrin overlays, one speaks of covered perforation. Penetration of an ulcer is called its penetration beyond the wall of the stomach or duodenum into adjacent organs. Ulcers of the posterior wall of the stomach and the posterior wall of the duodenal bulb usually penetrate and more often into the lesser omentum, the head and body of the pancreas, into the hepatoduodenal ligament, less often into the liver, transverse colon, gallbladder. Penetration of a stomach ulcer in some cases leads to the digestion of an organ, such as the pancreas.
Complications of an inflammatory nature include peri-ulcerous gastritis and duodenitis, perigastritis and periduodenitis, resulting in the formation of adhesions with neighboring organs. Rarely, a stomach ulcer is complicated by phlegmon. Severe complications of the ulcer are caused by Pyloric cicatricial stenosis. The stomach expands, food masses are retained in it, vomiting is often present. This can lead to dehydration, chloride depletion and the development of chlorohydropenic uremia (gastric tetany). Sometimes the scar pulls the stomach in the middle and divides it into two halves, giving it an hourglass shape.
In the duodenum, cicatricial stenosis and deformities are more often caused by ulcers of the posterior wall of the bulb. Malignancy of chronic stomach ulcers occurs in 5-10% of cases. One of the varieties of ulcerated stomach cancer develops from a chronic ulcer, or ulcer-cancer.
Transition of chronic duodenal ulcer into cancer - exclusively a rare event... Among the combined complications, the most common are perforation and bleeding, bleeding and penetration.
Peptic Ulcer Symptoms
Peptic ulcer disease is a chronic cyclical disease in which remissions are replaced by exacerbations. The onset of the disease in some patients is acute and the first clinical manifestations coincide with the formation of an acute ulcer. However, in most patients it is possible to establish a previous complex of subjective manifestations and functional and morphological disorders in the gastroduodenal system, which is usually characterized as a pre-ulcer state.
Pre-ulcer condition. This is the most controversial period of the disease. There are two types of pre-ulcer conditions:
- functional stomach upset of the hypersthenic type;
- chronic antral erosive gastritis, duodenitis, gastroduodenitis with normal and increased secretion.
During the observation of patients with developed ulcers in the outlet of the stomach or in the duodenum, they complained for a long time of pain in the epigastric region at night and on an empty stomach, they had local pain in the pyloroduodenal zone on palpation of the abdomen, high gastric secretion on an empty stomach and in the period between doses food, hyperchlorhydria of gastric juice and increased secretion of pepsin in all phases of digestion, accelerated indiscriminate evacuation from the stomach, accelerated passage in the duodenum, duodenostasis, prolonged decrease in antroduodenal pH. However, in these cases, unrecognized gastroduodenal ulcers cannot be ruled out.
Along with the pre-ulcer state, it is advisable to highlight the acute (initial) form of peptic ulcer disease, since at this stage it is most likely to achieve the patient's recovery and prevent complications.
Acute (initial) form of peptic ulcer disease. The acute form of the disease is usually regarded as the onset of chronic peptic ulcer disease. Criteria for the acute (initial) form of peptic ulcer disease:
- short history (up to 1-2 years);
- acute onset of the disease with a rapidly growing ulcerative symptom complex;
- fast (in the first 5 days) effect of the treatment;
- small (up to 0.4 cm) size and depth of the ulcer with moderate, in most cases limited inflammatory changes in the gastroduodenal mucosa;
- scarring of the ulcer within 20-25 days;
- absence or presence of minor cicatricial changes after the healing of the ulcer.
Single acute ulcers of typical localization (lesser curvature and outlet of the stomach, duodenal bulb) in the next 2-3 years recur in 30-35% of cases and therefore they should be considered as the initial stage of chronic peptic ulcer disease. Acute ulcers can also form as an episode in stressful situations, taking non-steroidal anti-inflammatory drugs. More often these are multiple ulcerations (acute ulcers, erosion), localized in the antrum of the stomach.
With the isolation of the pre-ulcer state and acute form peptic ulcer disease, it is necessary to take into account that stomach and duodenal ulcers can heal without the formation of a visible scar, in addition, an asymptomatic course of the disease is possible. These facts indicate how cautious one should treat the assessment of the initial stages of the development of peptic ulcer disease.
To understand the diverse manifestations of the disease, it is advisable to clearly outline the typical clinical symptoms of peptic ulcer disease.
A typical clinical picture. The main symptom in the clinical picture of peptic ulcer disease is pain. Pain syndrome is not only the main complaint of patients, but also often allows an accurate diagnosis of the disease without additional research methods, and sometimes contrary to their results. Pain in peptic ulcer disease has a clear rhythm (time of onset and connection with food intake), periodicity (alternation of pain with periods of their absence) and seasonality of exacerbations. It is characteristic that pain in peptic ulcer disease decreases or disappears after eating, antacids, anti-cholinergic drugs, and also after vomiting.
In relation to the time elapsed after a meal, it is customary to distinguish between early, late, "hungry" and night pains.
Early pains appear 0.5-1 hours after eating, their intensity gradually increases, lasts for 1.5-2 hours and decreases as the gastric contents are evacuated. Early pain is characteristic of ulcers located in the upper stomach. For ulcers of the antrum of the stomach and duodenal ulcers, late pains occurring 1.5-2 hours after eating, as well as "hungry" pains, are characteristic. "Hungry" pains are called because they occur after a significant period of time (6-7 hours) after eating and stop when it is taken. Close to "hungry" are night pains, which also decrease after eating.
A distinctive feature of peptic ulcer disease is the frequency of occurrence of pain syndrome. The periods of exacerbation usually last from several days to 6-8 weeks and are followed by a phase of remission. During remission, patients often feel practically healthy, even without following any diet.
Exacerbations of peptic ulcer disease, as a rule, are seasonal in nature, for middle lane this is mainly the spring or autumn season.
Pain in peptic ulcer disease is not clearly localized, there are aching, boring, cutting, cramping. In 50% of patients, pain is mild, dull, but in a third of cases it is very intense, sometimes reminiscent of pain in acute surgical abdominal diseases. Localization of pain in peptic ulcer disease is different and is usually determined by the location of the ulcer. It is noted that when the ulcer is located on the lesser curvature of the stomach, pain often occurs in the epigastric region, with pyloric and duodenal ulcers - in the epigastric region to the right of midline... With ulcers of the cardiac stomach, atypical localization of pain behind the sternum or to the left of it is often observed, and with postbulbar ulcers - in the back or in the right subscapularis.
The disappearance of pain after taking antacid, anticholinergic and antispasmodic drugs, as well as subsiding of the pain syndrome within the 1st week of adequate treatment are a characteristic differential sign of an uncomplicated form of peptic ulcer disease.
Violation of the typical "ulcerative" rhythm of pain, their resistance to treatment and the appearance of pain irradiation often indicate complications of peptic ulcer disease or the addition of concomitant diseases.
The pathogenesis of pain in patients with peptic ulcer disease has not yet been fully studied. Apparently, the mechanism of pain occurrence can be different. According to a widespread version, pain in peptic ulcer disease appears under the influence of an increased concentration of hydrochloric acid on the exposed sympathetic nerve endings at the base of the ulcer crater. This assumption is confirmed by the onset of a typical pain syndrome when irrigating an ulcer with 0.1 normal solution of hydrochloric acid through an endoscope, as well as quick elimination pain after taking antacids and significant relief of the condition of patients after vomiting. However, based on this concept, it is impossible to explain the often observed typical "ulcerative" pain in the absence of a gastroduodenal ulcer in the patient. Another cause of pain in peptic ulcer disease is considered to be movement disorders of the stomach and duodenum. A similar mechanism of pain syndrome is well traced in X-ray examination. It was shown that typical pains appear with pylorospasm and spasm of the initial sections of the duodenum, which are accompanied by a sharp increase in pressure in the stomach and increased motor activity. This point of view is consistent with the known analgesic effect of anticholinergic and antispasmodic agents. A certain participation in the pathogenesis of pain in peptic ulcer disease is attributed to other factors: ischemia of the mucous membrane due to vasospasm around the ulcer or their compression during spastic contraction of smooth muscles; reducing the threshold of pain sensitivity with inflammatory changes in the mucous membrane. In addition to pain, various dyspeptic disorders are included in the typical clinical picture of peptic ulcer disease.
Heartburn is a common symptom of peptic ulcer disease and occurs in 30-80% of patients. Heartburn is often the equivalent of pain, acting in the same timing with food intake as pain. Heartburn can alternate with painful sensations or precede them for a number of years, and sometimes be the only symptom of peptic ulcer disease. It should be emphasized that heartburn is not pathognomonic for peptic ulcer disease and is very common in cholelithiasis, chronic pancreatitis, gastroduodenitis and is one of the main manifestations of cardiac esophageal sphincter insufficiency. Main role the origin of heartburn is played by increased sensitivity of the esophageal mucosa to the peptic action of gastric contents and mechanical stretching of the esophagus by a wave of gastroesophageal reflux.
Belching- a nonspecific symptom that occurs in at least 50% of patients with peptic ulcer disease. In the occurrence of eructation, the main importance is also attached to cardia insufficiency in combination with antiperistalsis in the stomach. Predominantly sour belching is observed, which may be accompanied by regurgitation and salivation.
Nausea and vomiting are also characteristic symptoms of an exacerbation of peptic ulcer disease. Nausea is more often combined with vomiting. Vomiting in patients with peptic ulcer disease has some specific features. It occurs at the height of pain, being a kind of culmination of pain syndrome, and brings significant relief. Often, to eliminate pain, patients themselves artificially induce vomiting. Vomit is usually acidic in content, with a slight admixture of recently eaten food. In the mechanism of such vomiting, an increase in the tone of the vagus nerve is of primary importance, leading to sharp disturbances in gastric secretion and motility.
Appetite with a peptic ulcer, it is usually preserved or even increased. Decreased appetite in uncomplicated form of the disease occurs, as a rule, only with severe pain syndrome. More often than a decrease in appetite with an exacerbation of peptic ulcer disease, sitophobia is observed, that is, fear of eating due to the possibility of the onset or intensification of pain. Decreased appetite and sitophobia can lead to significant weight loss of the patient.
Constipation occur in almost 50% of patients with peptic ulcer disease. They usually intensify during periods of exacerbation of the disease and are sometimes so stubborn that they bother the patient even more than the pain itself. Constipation in peptic ulcer disease is due to a number of reasons: reflex dyskinesia with spastic contractions of the intestine of vagal origin, a sparing diet, poor coarse fiber that stimulates the intestines, restriction of physical activity, as well as taking certain medications (calcium carbonate, aluminum hydroxide, etc.). Peptic ulcer diarrhea is not typical, however, with prolonged constipation, irritation and inflammation of the colon can join, which is manifested by alternating constipation and diarrhea.
Thus, peptic ulcer disease is characterized by alternation of periods of exacerbations, when the listed symptoms are observed, and periods of remission. In the normal course, periods of exacerbation of duodenal ulcer continue for 4-8 weeks, and in case of gastric ulcer 6-12 weeks and end with the complete disappearance of clinical manifestations of the disease and scarring of ulcers. The duration of periods of remission ranges from several months to many years. Recurrence of the disease can be caused by mental and physical stress, gross error in food, taking certain medications (salicylates, corticosteroids, etc.), infection, sun exposure.
The given typical clinical picture of peptic ulcer disease is very schematic, in fact, the manifestations of the disease are very diverse and depend on the localization of the ulcer, its morphological characteristics, gender and age of the patient, as well as complications that have joined.
Ulcer of the lesser curvature of the body of the stomach. The majority of domestic and foreign scientists, using the term "gastric ulcer" without specifying the section of the lesion or "mediogastral ulcer", essentially mean this very localization of the ulcer. The ulcer of the lesser curvature of the body of the stomach is the most frequent localization of gastric ulcers and occurs in 36.8-68% of all its ulcerative lesions.
The age of patients with mediogastric ulcer usually exceeds 40 years, and among them there are many elderly and even old people. The clinical picture of ulcers of this localization is very diverse. The most common pains are noted in the epigastric region and somewhat to the left of the midline, arising 1-1.5 hours after eating and stopping after the evacuation of food from the stomach. Late, "hungry" and nocturnal pains are also observed. Pain sensations, as a rule, are aching in nature and are of moderate intensity. With ulcers of this localization, dyspeptic disorders (heartburn, nausea, rarely vomiting) are often found, in 30% of patients, appetite decreases and weight loss develops.
Bleeding complicates ulcers of the lesser curvature of the body of the stomach in 13.9% of cases, perforation - in 3.9%. It is believed that, on average, about 8-10% of benign mediogastric ulcers develop into cancer over time.
Ulcer of the greater curvature of the stomach. Rarely observed ulcers of the greater curvature of the stomach are among the ulcerative lesions of atypical localization and, according to various statistics, constitute from 0.2 to 4.6% of the number of ulcers of all localizations and up to 10% of stomach ulcers.
Among patients with peptic ulcer disease localized along the greater curvature of the stomach, men of older age groups predominate. There were no specific signs that distinguish her clinical picture from typical manifestations of peptic ulcer disease.
Interest in ulcers of large curvature is due not only to their rarity, but also to the fact that in 50% of cases they turn out to be malignant.
Antrum ulcer. Peptic ulcer disease with such localization is observed, according to summary data, in 10-16% of cases. An ulcer of the antrum of the stomach occurs mainly in young people.
The clinical picture of peptic ulcer disease with the localization of the process in the antrum is more similar to that of a duodenal ulcer than with ulcers of other parts of the stomach. Patients with pyloric ulcers are characterized by late, "hungry" night pains in the epigastric region. Along with the typical pain syndrome with ulcers of this localization, heartburn and vomiting of acidic gastric contents are often observed. Ulcers of the antrum of the stomach in 15-20% of cases are complicated by bleeding.
Currently, given the similarity clinical picture and pathogenesis, it is customary to consider ulcers of the antrum (pyloric) stomach and duodenal ulcers as a separate pyloroduodenal form of peptic ulcer disease.
Pyloric canal ulcers. Pyloric canal ulcers, according to various authors, are found in 2.1-7.8% of patients from all patients with peptic ulcer disease. The localization of the ulcer in the most narrowed part of the stomach, which carries a large functional load, determines the features of the clinical picture.
The main symptom of pyloric canal ulcers is pain. Pain syndrome mainly manifests itself in the following three variants:
- paroxysmal, severe pain lasting 20-40 minutes, repeatedly renewed during the day;
- gradually increasing and slowly subsiding severe pain;
- pains of moderate intensity, of varying duration, with a tendency to increase.
In almost 50% of patients, the onset of pain is not associated with food intake and in many there is no seasonality of exacerbations. However, in 30% of patients, pain does not differ from those in peptic ulcer disease of the duodenal bulb.
Along with the pain syndrome with ulcers of the pyloric canal, nausea and vomiting are often observed, which are persistent and often lead to significant weight loss. Other symptoms include persistent heartburn, paroxysmal salivation, decreased appetite, a feeling of fullness and quick satiety after taking even a small amount of food. All these phenomena are explained by persistent violations of the secretory and motor functions of the stomach.
Ulcers of the pyloric canal must be strictly delimited from ulcers of the duodenal bulb, since they have a peculiar clinical picture and can become malignant, which is absolutely not characteristic of duodenal ulcers.
Ulcers of the duodenal bulb. Most often, the localization of the ulcer is found on the anterior wall of the duodenal bulb (in 32.4-49.6% of cases). With this arrangement of the ulcer, typical clinical symptoms are mainly observed. The most characteristic complication of the ulcer of the anterior wall of the duodenal bulb is its perforation. Up to 60-75% of all perforations are observed precisely at this localization of the ulcer, and in 20-25% of cases, perforation occurs suddenly as the first manifestation of peptic ulcer disease.
The clinical picture is more varied when the ulcer is located on the posterior wall of the duodenal bulb (17.5-28.5%), especially when it penetrates into the pancreas and hepato-duodenal ligament. At the same time, a pronounced pain syndrome is noted, sometimes acquiring a paroxysmal character unusual for the disease, which is often associated with an associated reactive pancreatitis. With the development of reactive pancreatitis, the intensity of pain increases, their localization and irradiation change. In addition, with this localization of the ulcer, spasm of the sphincter of Oddi, dyskinesia of the biliary tract and the development of the syndrome of "congestive gallbladder", characterized by a feeling of heaviness and pain in the right hypochondrium with irradiation to the right subscapularis, can be observed.
Outside bulbous ulcers. Ulcers located distal to the duodenal bulb are usually called postbulbar. They make up 1.4-7.2% of all gastroduodenal ulcers and differ in a peculiar clinical picture.
Extra-bulbous duodenal ulcers are more common in men aged 40-60 years, and the disease begins on average 5-10 years later than when the ulcer is localized in the bulb.
The clinical manifestations of postbulbar ulcers and duodenal bulb ulcers are very similar, however, postbulbar ulcers are distinguished by a more persistent course, a significant frequency and duration of exacerbations. Pain is detected in 93% of patients and is usually localized in the right upper quadrant of the abdomen, spreading under the right shoulder blade and into the back. They occur 3-4 hours after eating, sometimes they are paroxysmal and resemble hepatic or renal colic. The pains disappear after eating not immediately, as with a bulbar ulcer, but only after 15-20 minutes.
The course of peptic ulcer disease with ulcer localization in the postbulbar region is characterized by a significant incidence of various complications. Among them, the most frequent is bleeding, which occurs in 42.8-79% of patients. Intestinal bleeding usually manifests itself in the form of melena and, much less often, bloody vomiting. It is often the first and only manifestation of a postbulbar ulcer. In addition to bleeding, perivisceritis is observed in 91% of patients, ulcer penetration (43%), duodenal stenosis (23%), ulcer perforation is found much less frequently (6% of patients).
In some patients, the disease is complicated by the addition of obstructive jaundice. Violation of the outflow of bile can occur as a result of reflex spzam of the sphincter of Oddi (sphincter of the hepato-pancreatic ampulla) or compression of the terminal sections of the common bile duct by inflammatory periulcerous infiltrate and scar tissue. Occasionally, perforation of the ulcer into the gallbladder and ducts with the formation of choledocho- or cholecystoduodenal fistulas is observed.
Combined and multiple gastroduodenal ulcers. Combined ulcers are understood to mean not only simultaneous ulcerative lesions of the stomach and duodenum, but also a combination of an ulcer of one localization with cicatricial deformity of another localization. The frequency of combined ulcers of the stomach and duodenum, according to most authors, ranges from 2.5 to 15%; there are indications that combined ulcers are much more common.
The sequence of development of associated ulcers can be different. Most often, the first is a duodenal ulcer and only a few years later a stomach ulcer is found (in 59.3-93% of cases). In 22-32.2% of patients, ulcers in the stomach and duodenum are diagnosed at the same time, which is more typical for young patients (under 30 years of age). Most rarely (6-30% of observations), a stomach ulcer appears first, and only then a duodenal ulcer joins. The development of gastric ulcers in patients with duodenal ulcer disease is explained by antral stasis and duodenogastric reflux.
The clinical picture of peptic ulcer disease in the presence of multiple ulcers characterized by great variety manifestations: from asymptomatic to severe and persistent pain syndrome. There is a tendency of multiple gastro-duodenal ulcers to complications, slow scarring and frequent recurrence. However, often the clinical manifestations of multiple ulcers do not differ from those in patients with single gastric or duodenal ulcers.
The peculiarity of the ulcers themselves ( giant size, prolonged non-healing) has an adverse effect on the course of peptic ulcer disease,
Giant ulcers. Most researchers refer to giant ulcers as ulcerative lesions with a diameter exceeding 3 cm. The literature describes ulcers reaching a diameter of 5-7 cm or more.
Giant ulcers are predominantly located on the lesser curvature of the stomach, less often in its subcardial part and on the greater curvature, and very rarely in the duodenum, usually in its initial segment on the posterior wall. There is a variety of clinical manifestations, regardless of their location. More often, giant ulcers are accompanied by severe pain syndrome without a characteristic periodicity, in some cases the clinical picture does not differ significantly from the usual one. However, a latent course of the disease is often observed or ulcers make their debut as a complication (bleeding, perforation). Giant ulcers are characterized by rapidly increasing emaciation.
Giant gastroduodenal ulcers are prone to massive bleeding, penetration (usually into the pancreas), less often ulcer perforation is observed. Data on the malignancy of giant ulcers are contradictory.
Peptic ulcer diagnosis
- Clinical diagnostic criteria
A thorough analysis of clinical symptoms is of great importance in the diagnosis of peptic ulcer disease, since it allows one to suspect the disease and conduct a targeted examination of the patient.
Peptic ulcer disease is characterized by a cyclical course with exacerbations of the same type, usually in spring and autumn periods years, but along with the typical clinical picture, there are numerous variants of it, as well as painless forms of the course of peptic ulcer disease.
An important place in the diagnosis of peptic ulcer disease is an objective examination of patients.
General inspection provides little information. Signs such as asthenic body type, facial expressions (accentuated nasolabial folds, sunken cheeks, deep forehead wrinkles), weight loss, pallor skin currently do not attach special diagnostic value. Attention should be paid to postoperative scars of the anterior abdominal wall, hyperpigmentation of the skin in the epigastric region as a result frequent use heating pad with severe pain syndrome. In thin people, it is sometimes possible to observe distinct undulating movements in the upper abdomen, which allows one to suspect pyloric stenosis.
In uncomplicated forms of peptic ulcer disease, the tongue is usually clean and moist. The covering of the tongue indicates concomitant diseases of the digestive system. With the development of complications of the disease, the tongue may become dry and thickly coated.
An objective examination of the abdomen provides valuable diagnostic symptoms. Local soreness and muscle protection of the abdominal wall in the epigastric region, as well as local irritation of the peritoneum (Mendel's symptom) are of some importance. Sometimes, with a jerky pressure on the abdominal wall, it is possible to feel the "splash noise". Its determination 7-8 hours after a meal (Vasilenko's symptom) indicates a violation of the evacuation of contents from the stomach due to pyloroduodenal stenosis or a pronounced hyperproduction of gastric juice. A vivid picture is observed with perforation of a stomach ulcer or duodenal ulcer (board-shaped abdomen, signs of peritonitis).
- Diagnostic value of laboratory tests
Study of gastric secretion. The study of gastric secretion in patients with peptic ulcer is important not so much for the diagnosis of the disease, but for the identification of functional disorders of the stomach caused by a disorder of neurohumoral regulation and structural changes in the glandular apparatus.
The state of acid secretion is determined by the method of fractional sounding of the stomach and intragastric pH-metry. Each of these methods carries Additional information and should be used depending on the problem being solved.
Numerous publications have been devoted to the determination of indicators of hydrochloric acid secretion during fractional gastric intubation in healthy people.
Analysis of the acid-forming function of the stomach in patients with duodenal ulcer showed that only 30-45% of the debit of basal and stimulated secretion of hydrochloric acid exceeds upper bound norms. The diagnostic value of the study of the secretory function of the stomach decreases due to the frequent detection of a hyperacid state in healthy people and the possibility of developing peptic ulcer disease with low acidity of gastric juice.
However, a significant increase in the acid-forming function of the stomach is more likely to indicate a peptic ulcer with pyloroduodenal localization.
In patients with peptic ulcer with localization of the process in the stomach, especially with mediogastric ulcers, a normal or slightly reduced flow rate of basal and acid-stimulated production is most often found.
Difficulties for interpretation arise when achlorhydria is found in a patient with peptic ulcer disease. In these cases, it is necessary to prove its true nature, which, however, is rarely done. To confirm true achlorhydria, a maximum histamine test or an intragastric pH-metry method is used.
The method of intragastric pH-metry has certain advantages over fractional gastric intubation. It allows you to identify the true anacidity, to determine the pH of the environment in different points stomach and duodenum, to evaluate differentially the reaction of the glands of the acid-producing zone to the effect of stimulants or secretion blockers. The method of intragastric pH-metry is physiological, since it excludes the traumatic process of aspiration, avoids technical errors caused by inaccurate titration and insufficient sensitivity of indicators. Intragastric pH metering is usually easier on patients and takes less time.
Usually, a probe with two sensors is used to register the pH of the body and the antrum of the stomach.
Most often in case of duodenal ulcer, pH-metry of the stomach reveals high hyperacidity with continuous acid production and decompensation of alkalization of the medium in the antrum.
According to intragastric pH-metry, with gastric localization of ulcers in most patients, continuous acid production of increased or moderate intensity is detected, but the alkalizing function of the pyloric region is usually preserved.
The use of pH-metry allows not only to clarify the nature of gastric acid secretion, but also to conduct pharmacological tests to identify indications for vagotomy in duodenal ulcer localization and to assess the effect of drugs on the secretion of hydrochloric acid in the stomach.
When selecting patients with peptic ulcer disease for selective proximal vagotomy, a test with atropine should be performed. After registering the pH of the basal secretion, the patient is injected subcutaneously with 1 ml of a 0.1% solution of atropine and the pH is measured for 1 hour. A sharply positive reaction, in which one can hope for a good effect after vagotomy, is considered to be an increase in pH by more than 4 units. With atropine-resistant hyperacidity, the pH changes by less than 0.5 units.
The disadvantage of the method of intragastric pH-metry should be attributed to the impossibility of determining the volumetric indicators of secretion, and therefore, to calculate the production rate of hydrochloric acid, therefore, pH-metry cannot completely replace fractional gastric intubation.
Pepsin plays an important role in the aggression of gastric juice. In patients with duodenal ulcer, a distinct increase in the level of proteolytic enzymes in gastric juice is usually observed. However, due to the wide individual range of fluctuations in the indicators of proteolytic activity of gastric contents, the diagnostic value of these methods is low.
Other laboratory research methods. A clinical blood test for uncomplicated forms of peptic ulcer disease remains normal. Occasionally, in patients with duodenal ulcer disease, erythrocytosis can be observed, due to an increase in erythropoiesis in the bone marrow under the influence of increased formation of an internal antianemic factor. When obvious or long-term hidden (occult) bleeding occurs from gastroduodenal ulcers, anemia develops, sometimes quite significant. Dynamic control over the level of hemoglobin in blood should be carried out in patients with peptic ulcer and without signs of exacerbation of the disease due to the possibility of its latent course.
The analysis of feces for occult blood has a certain diagnostic value. A positive reaction of feces to occult blood is often observed with exacerbation of peptic ulcer disease, however, the absence of positive results of this reaction does not reject the diagnosis of the disease and does not testify against its exacerbation, and a positive reaction to occult blood can also be detected in some other diseases: tumors of the gastrointestinal tract, nosebleeds, bleeding gums, hemorrhoids, etc.
Clinical and laboratory research allow only to suspect a peptic ulcer in a patient, while the methods that confirm the diagnosis are X-ray and endoscopic. These methods complement each other, therefore, for rational and optimal use, it is necessary to know their diagnostic capabilities.
- X-ray diagnostics
The most common method for diagnosing peptic ulcer disease is X-ray examination of the upper gastrointestinal tract. It is customary to distinguish direct and indirect symptoms of peptic ulcer disease. In the group of indirect symptoms, morphological and functional signs are distinguished.
Finding a "niche" is a direct sign of a peptic ulcer. Ulcerative "niches" can be of various sizes and have various shapes: round, oval, slit-like, conical, irregular, etc. A characteristic sign of ulcer penetration is an additional shadow of a suspension of barium sulfate next to the silhouette of the organ and three-layering in the ulcer "niche" (barium suspension, liquid, air). A modern, correctly performed X-ray examination allows you to identify an ulcer up to 2-3 mm in size.
Indirect functional symptoms of peptic ulcer disease include hypersecretion, change in evacuation (delay or acceleration of the passage of barium sulfate), duodenal reflux, duodenal dyskinesia, dysfunction of the cardia (cardiac insufficiency, gastroesophageal reflux esophagitis, hiatal hernia) spasms, changes in peristalsis (stenotic, deep, aperistaltic zone), changes in tone (hypotonia, hypertonicity). Indirect X-ray morphological signs are convergence of folds, cicatricial deformity of the organ.
- Endoscopic diagnostics
Gastroduodenoscopy with a flexible endoscope (fiberscope) is currently the most reliable method, allowing, with rare exceptions, to confirm or reject the diagnosis of peptic ulcer disease. Modern endoscopic examination not only reveals the ulcer defect, but also provides reliable control over its healing, and targeted biopsy allows you to assess the nature of changes in the mucous membrane at the edge of the ulcer, in the periulcerous zone and guarantees the accuracy of the diagnosis at the morphological level; medical procedures (stopping bleeding, local treatment of ulcers), as well as some functional tests, can be carried out through the endoscope.
Peptic ulcer treatment
In no other disease have so many medicinal and non-medicinal methods of treatment been proposed as in peptic ulcer disease, and all the authors note the effectiveness of the proposed methods. Their very abundance speaks of the absence of ideal means of therapy for this disease. Only the method of treating peptic ulcer disease can be considered effective, which quickly eliminates the symptoms of exacerbation, ensures active healing of the ulcer without unwanted side effects, and also prevents the development of a relapse of the disease.
It is necessary to very carefully evaluate the results of treatment and prevention, since peptic ulcer disease is a chronic cyclic disease, relapses of which may be asymptomatic, and ulcer healing occurs spontaneously and without treatment. Very few therapies for peptic ulcer disease have proven effective when studied in double-blind, placebo-controlled and endoscopic-guided studies.
Given the variety of etiological factors and the complexity of the pathogenesis of ulcerative disease, one cannot expect that a positive result can be achieved with the help of any one method of treatment. Treatment of peptic ulcer disease at all stages should be comprehensive and begin with general measures.
If possible, the causes that contribute to the onset and progression of peptic ulcer disease should be eliminated: stressful effects, smoking, taking alcoholic beverages and drugs with side ulcerogenic effects (acetylsalicylic acid, indomethacin, reserpine, corticosteroid drugs, etc.).
Modern therapy of peptic ulcer disease should be pathogenetically substantiated and aimed at reducing the aggressiveness of gastric and duodenal contents, at normalizing gastric and duodenal motility with suppression of duo-denogastric reflux, at increasing protective properties mucous membrane, as well as the restoration of impaired neuro-humoral regulation of the functions of the gastroduodenal system.
In the treatment of patients with uncomplicated forms of peptic ulcer disease, three stages are distinguished:
- antiulcer therapy during an exacerbation of the disease, aimed at eliminating the clinical manifestations of the disease and accelerating the healing of ulcers;
- rehabilitation treatment (rehabilitation after the healing of the ulcer);
- preventive measures to prevent relapse and lengthen remission. With complicated forms of the disease, it is often necessary to resort to surgical methods of treatment.
Conservative treatment
- Exacerbation treatment
During the period of exacerbation of peptic ulcer disease, complex treatment should be carried out. All treatment methods can be divided into pharmacotherapeutic and non-pharmacological.
Mode. There are two points of view on the need for hospitalization and adherence to a strictly limited regimen for patients during an exacerbation of peptic ulcer disease.
Until recently, hospitalization was considered compulsory. In the hospital, they were prescribed strict bed rest for 2 weeks, from 3-4 weeks they were allowed to get up for 2-3 hours during the day. The feasibility of such an approach was based on a more rapid relief of pain syndrome, a reduction in the time for scarring of ulcers, and also on the need to save energy due to the low calorie intake of diet 1a and 1b, which patients received in the first 3-4 weeks.
In recent decades, there have been publications on research in which it was not established significant differences in the effectiveness of inpatient and outpatient treatment of patients. The data obtained made it possible to raise the question of the possibility of treating patients with exacerbation of peptic ulcer on an outpatient basis, and in some cases with continuation labor activity.
According to foreign researchers, hospitalization does not increase the effectiveness of antiulcer therapy, and patients with uncomplicated peptic ulcers do not need bed rest and should be treated on an outpatient basis, without interrupting their work.
Diet. Diet remains an important component of peptic ulcer treatment. However, the views on nutritional therapy in this disease for last years have undergone significant changes.
The main idea of diet therapy was that a certain set of products, a way culinary processing food and diet can accelerate ulcer healing. The ways of realizing this effect were associated with the ability of a certain food composition to suppress the secretion of hydrochloric acid, inhibit motility, protect the mucous membrane from the action of damaging factors, and provide the body with a sufficient amount of nutrients it needs. To achieve these goals, a large number of diets have been proposed based on the principles of chemical, mechanical and thermal sparing of the gastrointestinal tract and an increase in the rhythm of food intake.
Currently, the Institute of Nutrition of the Russian Academy of Medical Sciences has developed a new antiulcer diet with increased content protein (125 g) and fat (130 g). The reason for the introduction of the new diet was that with an increase in the proteins and fats supplied with food, the regeneration processes are enhanced, the production of hydrochloric acid decreases, the motor-evacuation function of the stomach is normalized, which has a beneficial effect on the healing of ulcers.
When prescribing therapeutic nutrition for peptic ulcer disease, one should also take into account the presence of concomitant diseases of the digestive system and individual intolerance to certain foods, such as milk.
Physiotherapy. For the treatment of patients with peptic ulcer disease, a large number of various physiotherapeutic methods have been developed and introduced into clinical practice.
The most effective are thermal procedures (heating pads, poultices, warming compresses, mud, paraffin and ozokerite applications). For the same purpose, decimeter therapy (UHF) is used. Heat relieves smooth muscle spasm, normalizes gastrointestinal motility and improves blood flow to the mucous membrane. All this contributes to the elimination of pain and healing of the ulcer. Heat treatment is contraindicated in complicated forms of peptic ulcer disease, as well as in suspected malignant ulceration.
With severe pain syndrome, they found wide application sinusoidal modulated currents (SMT), the analgesic effect of which is associated with the normalization of motor-secretory disorders in the gastroduodenal system.
In recent years, intraorgan electrophoresis with various drugs has been used. In this case, the patient takes a solution of the necessary drug inside, and then galvanization is performed. Antispasmodic drugs (no-shpa, papaverine) are used, and aloe is used to stimulate regeneration.
Magnetic therapy has become widespread in the treatment of patients with peptic ulcer, especially in the presence of concomitant diseases (chronic pancreatitis, cholecystitis, etc.). It is well tolerated by patients and has an undeniable therapeutic effect. As a result of the use of magnetotherapy, pain syndrome and dyspeptic disorders are quickly relieved.
Patients with severe functional disorders of the nervous system are shown hydrotherapy in the form of therapeutic showers, pine, oxygen and pearl baths. A positive effect in these cases is also achieved by the appointment of electrosleep, central (cerebral) electroanalgesia.
Physical treatments include hyperbaric oxygenation. A prerequisite for the use of oxygen therapy is the important role of local ischemia of the mucous membrane of the stomach and duodenum in ulceration.
Psychotherapy. Psychotherapy in the treatment of patients with peptic ulcer disease is clearly underestimated, although it is well known that the disease often develops with certain psychological characteristics personality and after emotional stress. The method of psychotherapy can be easily mastered by both a gastroenterologist and a general practitioner. The doctor should identify traumatic factors, establish temporary connections between stressful situations and the onset of the disease, be informed about the patient's lifestyle, family and work relationships. This allows you to better understand the patient and provide him with psychological support, which ultimately can have a positive effect on the outcome of the disease.
Pharmacotherapy of peptic ulcer disease. Drug therapy is the main component in the treatment of peptic ulcer disease exacerbation. Over the past 10-15 years, the arsenal of antiulcer drugs has been replenished with new active drugs.
All pharmacotherapeutic agents used in the treatment of peptic ulcer disease can be divided into three large groups:
- locally acting agents aimed at suppressing the aggressive properties of gastric contents;
- drugs that increase the protective properties of the mucous membrane;
- affecting the central neurohumoral regulation of the gastro-duodenal system. Such a division is very arbitrary, since many drugs can simultaneously act on various pathogenetic links of ulceration.
Rehabilitation of patients should begin from the moment of primary detection of peptic ulcer disease or its recurrence and should be aimed at achieving stable remission and restoration of structural and functional disorders of the gastroduodenal system.
Rehabilitation of patients with peptic ulcer disease in the acute phase is usually carried out in a hospital. However, at present, there is a tendency towards an individual choice of the place of treatment, taking into account the characteristics of the course of the disease, lifestyle, work, personality traits the patient, his attitude to the proposed conditions of treatment. The goal of restorative treatment in this phase of the disease is to achieve the fastest healing of the ulcer and the maximum normalization of morphological and functional disorders in the gastroduodecal system. As practice shows, the average time for scarring a duodenal ulcer is 25-30 days, for a stomach ulcer - 40-45 days. During these periods, as a rule, a fresh ("red") scar is formed, but signs of active gastroduodenitis remain.
The phase of subsiding exacerbation lasts 3-6 months, and rehabilitation treatment continues under the supervision of doctors of the polyclinic (outpatient stage). During this period, patients, even with uncomplicated peptic ulcer disease, are recommended to follow a diet for 3-4 months, as well as to carry out supportive drug therapy for 1-1.5 months. For maintenance treatment, it is advisable to use such affordable, easy-to-use and practice-tested complex drugs such as vikalin, vikair, as well as almagel, phosphalugel.
Surgery
Indications for surgical treatment of peptic ulcer disease are usually divided into absolute and relative. Absolute indications include:
- perforation of the ulcer;
- profuse gastrointestinal bleeding;
- stenosis of the duodenum or the outlet of the stomach with impaired evacuation function;
- malignancy of the ulcer (most often gastric localization).
Relative indications for surgical treatment of ulcers are:
- ineffectiveness of conservative therapy, adequate in terms of the selection of medicines and the duration of treatment;
- history of repeated profuse gastrointestinal bleeding;
- relapse of the disease after suturing a perforated ulcer; large callous penetrating ulcers, resistant to drug treatment.
Treatment of patients with severe complications of peptic ulcer disease is only surgical, and only in case of gastrointestinal bleeding, along with the operation, complex hemostatic therapy can be used, including various endoscopic methods for stopping bleeding.
Unfortunately, many clinicians define the indications for surgical treatment in different ways when drug therapy is unsuccessful. Sometimes patients have to undergo treatment in various hospitals for years, despite the annual exacerbation of the disease, and doctors do not think about the advisability of referring them to a surgeon. Such a long-term therapeutic treatment without significant success in achieving long-term remissions significantly increases the risk of severe surgical complications in this category of patients. Apparently, there is no need to prove the indisputable truth that surgical intervention performed in case of complications of peptic ulcer disease, when the patient's life is on the brink of disaster, presents an incomparably higher risk than an operation performed in a planned manner against the background of complex preoperative preparation. It remains only to regret that in our country, almost half of all surgical interventions are performed according to absolute indications. Wider application planned operations according to relative indications, it would significantly reduce postoperative mortality, that is, save many hundreds of human lives.
In addition, more favorable long-term results of surgical treatment of peptic ulcer disease are noted in the absence of gross morphological and functional changes in various organs. digestive system and above all the pancreas, liver and gallbladder. Therefore, a significant delay in performing the operation according to relative indications to a certain extent reduces its effectiveness.
Obviously, it can be concluded that if 3-4-fold inpatient treatment, adequate in terms of timing and selection of medications, does not lead to the patient's cure or the achievement of sufficiently long clinical remissions, the referral of the patient to surgical treatment is justified.
Failure of drug therapy, performed inadequately in terms of the selection of drugs, on an outpatient basis and in violation of the duration of the course of treatment (less than 3-4 weeks) without endoscopic control of its effectiveness, is not an indication for surgical treatment, since this category of patients is far from the possibilities and reserves of complex therapeutic treatment have been exhausted.
A patient's history of several profuse gastrointestinal bleeding indicates an aggressive course of the disease, therefore, even if the patient has not previously been adequately treated therapeutically, it is necessary to raise the question of the expediency of surgical intervention.
Clinical observations show that after suturing of perforated ulcers, 50-80% of patients subsequently develop a relapse of peptic ulcer disease, and most of them have even the most modern drug treatment has very mediocre results. Therefore, the failure of even 1-2-fold therapeutic treatment of ulcers that recur after this operation should be recognized as an indication for surgical treatment.
With large, callous, penetrating ulcers, the effectiveness of conservative treatment is usually low, while the risk of developing severe complications and pronounced changes from nearby organs is very high. In such situations, surgical treatment is more promising.
The above indications for surgery are common for patients with both gastric and duodenal ulcers. Nevertheless, given the rather high incidence of malignancy of gastric ulcers, in this category of patients, the relative indications for surgery should be expanded.
Contraindications to surgical treatment of peptic ulcer disease are various severe diseases of internal organs with decompensation of their functions. With severe complications of peptic ulcer disease (perforation, bleeding, stenosis, malignancy), the range of contraindications for surgery (especially for emergency) is sharply narrowed and limited only to those situations when the risk of surgery seems to be excessively high (acute traumatic myocardial infarction, acute stroke, etc.). Due to the current use of low-traumatic organ-preserving operations with vagotomy, as well as the success of anesthesiology and resuscitation, contraindications to planned surgical treatment can also be significantly limited.
Stomach ulcer and duodenal ulcer have certain differences in etiology, pathogenesis and clinical course, and therefore it is advisable to consider the problems of their surgical treatment separately.
Historically, the first and fairly widespread method of surgical treatment of duodenal ulcer is gastric resection. In this operation, 2/3 of the organ is removed, followed by the imposition of an anastomosis between the stump of the stomach and the initial part of the jejunum. Due to technical difficulties, it is much less likely to complete the operation by forming a gastroduodenal anastomosis. The main and, perhaps, the only advantage of gastric resection is a reliable cure of the patient from peptic ulcer disease. The recurrence rate is usually 1–2%.
The negative side it is relatively high postoperative mortality - about 3-5%. Considering that about 50,000 gastric resections are performed annually in our country, the number of deaths will be quite impressive. In addition, 15-30% of patients subsequently develop various post-gastro-resection syndromes (dumping syndrome, adductor loop syndrome, hypoglycemic syndrome, etc.), which are poorly amenable to drug and surgical treatment, leading many patients to disability. Somewhat less often, pathological syndromes are observed after gastric resection according to Billroth-1.
An alternative to gastric resection is vagotomy, performed in one form or another.
Stem vagotomy with gastric drainage operations is technically a relatively simple, low-traumatic intervention, the implementation of which takes a very short time. Among the operations that drain the stomach, the most often used are pyloroplasty according to Heineck - Mikulich, Finney or gastroduodenostomy according to Zhabula. Postoperative mortality during this operation usually does not exceed 1%. Various functional disorders on the part of the digestive system (dumping syndrome, diarrhea, etc.) develop less frequently than after resection of the stomach, and proceed in a milder form. The disadvantages of this operation should also include a fairly high frequency of recurrence of peptic ulcer disease; reaching 8-12% The main reason for the recurrence of the disease is insufficient inhibition of the acid-producing function of the stomach, which is associated with incomplete vagotomy (ie, technical errors in performing the intervention). The frequency of relapses can be significantly reduced due to the correct selection of patients for surgery and the improvement of the technique of performing vagotomy. The incidence of disability in patients after stem vagotomy with pyloroplasty is significantly lower than after resection of the stomach.
Quite often, especially in persons with excessively high rates of acid production, stem vagotomy is used in combination with economical gastrectomy. This operation allows you to reliably suppress gastric secretion and thereby significantly reduce the recurrence rate to 0-1%. Mortality usually does not exceed 1-2%, which is somewhat lower than after extensive gastrectomy. Various pathological syndromes after vagotomy with economical gastrectomy occur somewhat less frequently and proceed in a milder form than after classical resection of 2/3 of the stomach, and the incidence of disability is also somewhat lower.
In recent years, FPV has become especially widespread. The essence of this operation is parasympathetic denervation of the body and the fornix of the stomach (i.e., its acid-producing zone) while maintaining the innervation of the antral-pyloric region, which allows the intervention to be performed without additional manipulations on the stomach associated with the destruction of the pylorus. At the same time, the parasympathetic innervation of all organs of the abdominal cavity is preserved. Postoperative mortality with PWV is 0.3% on average, which is more than 10 times lower than with extensive gastrectomy. Various pathological syndromes are rare, and their severe forms are practically not observed. In this regard, the disability of patients is also very rare. The negative side of PWV is a relatively high recurrence rate - 5-10%. However, not all patients with recurrent ulcers after PWS are subject to reoperation. In many of them, the disease is asymptomatic or with minimal clinical manifestations, and adequately conducted conservative treatment has a fairly good and lasting effect. According to modern concepts, SPV is the method of choice in the surgical treatment of uncomplicated duodenal ulcers.
The Ministry of Health of the Russian Federation approved the drug Revolide (Eltrombopag) for use in children. The new drug is indicated for patients suffering from chronic immune thrombocytopenia (idiopathic thrombocytopenic purpura, ITP), a rare disease of the blood system.
03.03.2017
Canadian scientists from the University of Ottawa are set to revolutionize restorative medicine. In one of their latest experiments, they managed to grow a human ear from an ordinary apple.
27.02.2017
Specialists of the Pavlov First Medical University in St. Petersburg have created nanoparticles with the help of which it is possible to diagnose infarction and pre-infarction conditions of a patient. Also in the research perspective, nanoparticles will be used ...
Medical Articles
Almost 5% of all malignant tumors are sarcomas. They are characterized by high aggressiveness, rapid hematogenous spread and a tendency to relapse after treatment. Some sarcomas develop over the years, without showing themselves ...
Viruses not only float in the air, but they can also get on handrails, seats and other surfaces, while remaining active. Therefore, on trips or public places, it is advisable not only to exclude communication with people around you, but also to avoid ...
To regain good eyesight and say goodbye to glasses and contact lenses forever is the dream of many people. Now it can be made a reality quickly and safely. New possibilities of laser vision correction are opened by the completely non-contact Femto-LASIK technique.
Cosmetics designed to take care of our skin and hair may not actually be as safe as we think.
The pathogenesis of gastric ulcer and duodenal ulcer is manifested due to the formation of erosions and ulcers on the organs. As a result, patients develop pain syndrome, dyspeptic disorders - indigestion, heartburn, aching pains, heaviness in the stomach. If the ulcer is not treated, such neglect will lead to the formation of a hole in the stomach. As a result, the contents of the organ enter the body, often causing infection.
The etiology of peptic ulcer disease is explained by factors: depression, stressful conditions, poor material conditions, unhealthy diet.
The etiology and pathogenesis of peptic ulcer disease is expressed in a decrease in tolerance to traumatic situations that lead to the formation of a psychosomatic cycle.
A significant role is given to emotional overload, poor nutrition, and alcohol consumption. The pathogenesis of gastric ulcer occurs when the digestive process is disturbed, provoking the disease.
Some associate the pathogenesis of gastric ulcer and duodenal ulcer with impaired activity of the nervous system. But this point of view is not universal.
The causes of the onset of the disease are:
- the presence in the body of bacteria that cause ulcers - Helicobacter pylori;
- chronic duodenitis, gastritis;
- frequent use of medications;
- alcohol abuse.
The cause of the ulcer is nitrates
The cause of the appearance of an ulcer is the use of "wrong" products in a large number... Known carcinogens that provoke the appearance of ulcers are nitrates. Sodium nitrate is a carcinogen found in raw sausage. Salt becomes a carcinogen for the stomach, patients should limit the use of salty foods.
A stomach ulcer sometimes develops in a latent form, often appears on the basis of erosion of the walls of the stomach, gastritis. A person is not aware of the presence of the disease until the condition worsens. In order to prevent the appearance of stomach and duodenal ulcers, do not wait for the transition of the disease to another, treat the underlying disease and follow the doctor's recommendations.
Now a stomach ulcer is considered as a pathology that occurs due to disruption of the humoral, endocrine, and nervous systems. The etiology of peptic ulcer disease is associated with impaired activity of the autonomic and central systems. sometimes lies in the malfunctioning of the pituitary gland.
Symptoms of the disease
The leading symptom of the disease is prolonged pain in the abdomen or right hypochondrium. Especially frequent are autumn and spring exacerbations of a seasonal nature.
- Resection, as a result of the intervention, the ulcer is removed along with part of the stomach.
- Vagotomy, in which the food organ is preserved. The nerve endings responsible for the formation of the hormone gastrin, which provides digestion, are cut.
- Endoscopic method: a special laparoscopic technique is inserted into small holes, with the help of which the operation takes place.

Ways to prevent recurrence of the disease
In order to avoid relapse with the initial symptoms of this pathology, it is allowed to use folk methods treatment. Several groups are known medicinal plants... Before starting treatment, you need to understand the qualities of herbs.
Traditional methods of treating the disease:
- Herbs that activate the restorative function of digestion. Plants include aloe, dandelion, sea buckthorn.
- They activate the secretory function of the glands, regulate the gastric juice: tansy, pine buds, calamus, chamomile, peppermint.
Diet for stomach ulcers
Observing a diet, patients with a diagnosis should strictly adhere to the rules:
- Do not eat foods that provoke gastric secretions.
- Food is allowed boiled or steamed. You should not eat fried foods, especially meat with a hard fried crust.
- Portions are small for easy digestion. The break between meals is no more than three hours.
- Do not allow the use of hot or too cold food. Bring to normal temperature before eating.
- Limit salt intake. For patients with peptic ulcer, the consumption rate is known - 10 grams per day.
Food should be of high quality, healthy, rich in nutrients and minerals. The use of fermented milk products and milk - it is desirable to soften the gastric juice. The foregoing applies only to those patients who do not have milk intolerance. It is allowed to add tea or coffee to the product, but strong coffee is highly undesirable. Food is welcome olive oil, contributing to the rapid healing of wounds.
What foods can be included in the diet
The menu of patients diagnosed with gastric ulcer should contain the following foods:
- wheat bread;
- soups;
- eggs, steamed omelet;
- non-sour sour cream, milk, fresh cheese, cream;
- meat of chicken, veal, beef refined from fat, which is boiled or meatballs;
- fish with a low percentage of fat;
- beets, pumpkin, carrots, potatoes are used in the form of mashed potatoes or stews;
- cereals and pasta, which are rarely served on the table;
- vegetable and butter oil - no more than 100 grams per day;
- sweet berries - strawberries, blueberries, raspberries;
- sweet fruits that can be baked or grated;
- jellies, creams, jelly, compotes cooked from sweet fruits.
- sauces, such as bechamel;
- vitamins from freshly squeezed juice, decoction of wheat bran, rose hips.
What foods should be excluded from the diet
You can not drink strong mushroom, meat, fish decoctions. Eliminate animal fats from consumption. The heavy fiber from hard vegetables irritates the stomach.
Patients with ulcers are supposed to forget about spicy, salty, fried foods containing carcinogens. Soda water and drinks, chocolate products, canned food should be discarded.
Eat several small portions of food a day. Eat five to six times a day. The last meal is two hours before bedtime. If you correctly adhere to a diet, eat right, the attacks of peptic ulcer disease will decrease, and soon they will completely disappear.
How to prevent the appearance of a peptic ulcer
Stomach ulcers appear most often due to improper nutrition. This leads to increased acidity and ulcers. Frequent consumption of alcoholic beverages, smoking - become the cause of the disease. When the first symptoms appear, it is necessary to exclude harmful substances from the diet.
Nervous strain can lead to prolonged depression and stomach ulcers. To avoid this, you need to spare the nervous system, take care of emotional health.
A healthy way of life should be the foundation of human existence. This is the only way out that contributes to the full recovery of the body after an illness.
Peptic ulcer disease (PUD) is a chronic recurrent disease associated with the action of various exogenous and endogenous risk factors, the formation of pathogenetic reactions as a result of disturbances in the mechanisms regulating the morphofunctional state of the gastroduodenal zone, the clinical manifestations and complications of which are mainly due to the activity of the ulcerous process.
Peptic ulcer etiology. At one time, there was an opinion that ulcer develops mainly in persons with special type of neuro-endocrine shifts. It is believed that patients with ulcer are characterized by increased reactivity and sensitivity, instability of behavior, a tendency to autonomic disturbances, mood swings, poor tolerance of strong stimuli.
There are no clear connections between YaB and climatic features and racial identity of people.
Characterizing patients with ulcer, one cannot but dwell on factor of heredity. In clinical practice, there are cases when whole families and close relatives suffered from ulcer.
According to our research, hereditary predisposition in different years was detected in 13–38% of cases.
Hereditary predisposition to ulcer can be manifested by a genetically determined increase in the mass of the parietal cells in the gastric mucosa, combined with hyperactivity of its secretory apparatus, hypersensitivity of the parietal cells of the stomach to gastrin and histamine, increased production of pepsinogen-1, peculiarities of microcirculation and motility in the gastroduodenal zone. A.
Most gastroenterologists consider PU polyetiological disease. Among the etiological factors leading to the development of the disease and its relapses, there are alimentary, household and industrial hazards, medicinal effects, diseases of a number of internal organs, neuropsychic trauma, physical stress, Helicobacter pylori infection.
According to our data, irregularity of nutrition, inadequacy of food, errors in diet as contributing factors in the development of ulcer and its relapses were detected in 39.6% of patients.
Regarding the importance of alimentary and household factors in the development of PU, one cannot exclude the role of alcohol and tobacco smoking.
Ulceration in the gastroduodenal zone can occur against the background of the use of various medicines. So, the development of ulcers in the stomach and duodenum is known during treatment with aspirin, butadione, indomethacin, glucocorticosteroid hormones, reserpine, etc.
However, there are opinions that drug-induced gastroduodenal ulcers have nothing to do with ulcer, nevertheless, taking a number of medications can provoke relapses of the disease and its complications.
Contribute to the development and exacerbation of the disease industrial hazards, such as physical overload, work associated with severe vibration in hot shops, contact with vapors of alkalis and acids, ingestion of metal processing particles, pesticides, etc. with saliva.
It has long been noted that there are a number of diseases, which often accompany YaB. In this regard, the question of the relationship between nuclear weapons and chronic gastritis.
According to our observations, chronic gastritis occurred in 58.9% of men and 66% of women suffering from ulcer.
Clinical practice often shows a connection between an exacerbation of ulcer, and, in some cases, its first manifestations with psycho-emotional influences... The particularly important role of neuropsychic influences in the etiology of ulcer was pointed out in their works by K.M. Bykov and I.T. Kurtsin (1949, 1952). Based on the teachings of I.M. Sechenov about the reflex nature of the activity of the brain and I.P. Pavlov about cortico-visceral physiology and pathology, as well as the trophic influence of the nervous system, they put forward cortico-visceral theory of pathogenesis I WOULD.
Chr assigned a large role to the psycho-emotional factor in the etiology of ulcer. Brailski (1976). For example medical professionals he showed a relationship between the severity of neuropsychic overloads and the frequency of ulcer. Thus, it is 15-17% for doctors, 8.06% for nurses, and 3.9% for juniors.
There are a large number of reports indicating the connection of this suffering with diseases and trauma of various parts of the nervous system... Cases of the development of ulcers in the stomach and duodenum in persons with acute cerebrovascular accident, suffering from a tumor of the cerebellum, medulla oblongata, and thoracic spinal cord are presented. Surgical removal of the tumor in a number of patients led to the healing of the ulcer.
Selye (1952, 1960) comes to the conclusion that not only neuropsychic trauma, but also any stress factor can lead to a breakdown of the adaptive mechanisms of the body and cause the development of a pathological process, including ulcer.
After the discovery of Warren and Marshall (1983) pyloric campylobacter (Campylobacter pylori) which are currently referred to as Helicobacter pylori(HP), the question of the etiological role of these microorganisms in ulcerogenesis began to be widely discussed. There is evidence that in patients with duodenal ulcer, HP is isolated from biopsies of the antrum of the gastric mucosa in 82-100% of cases, and with gastric ulcer - in 50-70%.
For the first time, the idea of the important role of microorganisms in the development of ulcer was expressed in 1897 by A. Krupetskiy.
In 1925 Duval wrote: “We are not claiming that infection is the root cause of stomach ulcers. An ulcer, a wound on the gastric mucosa can appear under the influence of a wide variety of reasons: vascular, traumatic, chemical, thermal, and so on, but for it to acquire a chronic course, in order to pass into a specific stomach ulcer, this requires an infection. "
M.K. Dahl (1938) considered the microflora of the stomach as the cause of septic complications of ulcer.
Etiological significance in different time were given to various types and genera of microorganisms: staphylococci, streptococci, candida, Escherichia coli.
According to various authors, in patients with ulcer, microorganisms from the gastroduodenal zone were isolated up to 96.6% of cases. It is significant that microorganisms were sown from the unchanged mucous membrane in 5.3% of cases, from the gastritis zone around the ulcer - in 90.8%, and from the ulcer ridge - in 96.3%. The qualitative composition of the microflora included representatives of the genera Staphylococcus, Streptococcus, Miсrococcus, Neisseria, Lactobacillus, Escherichia, Klebsiella, Citrobacter, Proteus, Eubacterium, Pseudomonas, Corynebacterium, Bifidobacterium, Bifidobacterium, Bacteroides, Bifidobacterium. The frequency of isolation of Helicobacter pylory in PUD ranged from 40-62% to 100%.
According to our data (Egorova E.N., 1999; Chernin V.V., Chervinets V.M., Bondarenko V.M., Bazlov S.N., 2004), during the recurrence of ulcer, there was an excessive growth of mucous microflora in the stomach and the duodenum, especially pronounced in the periulcerous zone.
On average, more than 22 genera of microorganisms were isolated from mucosal biopsies. At the same time, the dissemination of the periulcerous zone of duodenal ulcers (28 genera and types) was greater than that of the stomach (15 genera). Staphylococci and streptococci were sown in almost 100% of cases, lactobacilli, enterobacteria, bacteroids, candida, micrococci in 70-40%, less often - other microorganisms. It should be noted that bacteria unusual for normal microbiocenosis were also isolated from mucosal biopsies.
In most cases (21-35%) microorganisms were isolated in the form of 4, 5 and 6 cultures, less often (in 10.5-2.6%) 7-10 cultures. Microorganisms were not isolated in monoculture.
Helicobacteria from biopsies of the mucous membrane of the periulcerous zone of gastric ulcers were inoculated in 16.7% of patients, and in the duodenum - in 33% of cases. In gastric ulcer, microorganisms were inoculated from the antrum of the stomach in 29.2% of patients, but they were not found in the fundus. In case of ulcer duodenal ulcer, they were isolated from these parts of the gastric mucosa in 23% and 14.3% of cases, respectively.
It is important to note that the microorganisms isolated during the recurrence of ulcer from the gastroduodenal zone had a wider range of enzymatic activity than mucous microflora of healthy people. In addition to urease, hemolysin, caseinase and RNAase, they produced lecithinase, plasma coagulase, catalase, and 70% of them acquired cytotoxicity, i.e., the ability to destroy epithelial cells.
This circumstance indicates that during the period of recurrence of ulcer in the gastroduodenal zone, dysbacteriosis is formed with excessive growth of mucosal microflora (pathomicrobiocenosis), enhancing inflammatory-necrotic changes in the mucous membrane.
The fact of rare detection of HP in the area of the ulcerative defect may indicate its doubtful leading role in the development of the ulcerous process. Therefore, in the treatment of recurrent ulcer, attention should be paid not so much to HP, but to the elimination of excessive growth of mucosal flora (pathomicrobiocenosis) and restoration of normobiocenosis.
Thus, the etiology of ulcer currently seems to be a complex and not fully understood problem. Etiological factors, with which the development of the disease is associated, can be divided into exogenous and endogenous, basic and predisposing.
TO exogenous factors should include:
1. Neuropsychic influences, psycho-emotional stress.
2. Injuries, diseases of the brain and their consequences.
3. Food inaccuracies, malnutrition, intolerance to certain foods (food intolerance).
4. Long-term use of drugs with ulcerogenic action.
5. Household and industrial hazards.
6. Meteorological conditions.
From endogenous factors most often distinguish:
1. Hereditary predisposition.
2. Features of the blood group.
3. Constitutional status.
4. Gender and age.
5. A number of diseases of internal organs, endocrine system, defects of the chewing apparatus.
6. Dysbacteriosis of the gastroduodenal zone.
A very difficult task is to identify the main and predisposing etiological factors. Based on the analysis of literature data and the results of our research, we join the opinion that the main etiological moments of ulcer are neuropsychic trauma, alimentary disorders and a number of other exogenous influences.
The predisposing etiological factors include hereditary and constitutional features, gender and age, and some diseases of internal organs.
All of the above indicates that ulcer should be considered as a polyetiological disease. This point of view is confirmed by the fact that the disease develops more often in men at a young age, often in persons with a burdened heredity, who do not follow the diet, have bad habits, are often exposed to neuropsychic overload and react violently to them.
Peptic ulcer pathogenesis. Discussing the pathogenesis of ulcer, one should dwell on two questions. The first is the mechanisms of the formation of gastroduodenal ulcers and the second is the pathogenesis of the disease itself, the causes of its chronic, recurrent course.
The formation of a peptic ulcer in the gastroduodenal zone occurs against the background of pronounced disorders of the secretory and motor-evacuation functions of the stomach, a decrease in various defense mechanisms her mucous membrane.
However, to date, the issue has not been finally resolved. where does the formation of the ulcerative process come from?- from the surface of the mucous membrane or from the inside? A number of researchers believe that the development of an ulcer begins with damage to the surface layer of the mucous membrane, with a breakthrough of the mucous-bicarbonate-epithelial barrier at the site of focal gastritis or duodenitis, associated with the action of various etiological factors, including Helicobacter pylori.
Our long-term clinical observations and experimental studies have shown that ulceration is based on focal microcirculation disorders in the mucous membrane of the gastroduodenal zone.
An equally important problem when discussing the pathogenesis of the disease is to find out trigger mechanism or the main primary pathogenetic moment, leading to the subsequent inclusion of various pathogenetic factors that form the ulcerative process.
Considering that psycho-emotional stress and other influences that injure the nervous system are one of the common causes of ulcer disease and its relapses; visceral and neuro-endocrine connections, the emergence of microcirculatory, secretory and trophic disorders in the gastroduodenal zone.
Our long-term clinical observations have shown that various disorders of nervous regulation occurred in 88.9% of the examined patients and only 11.1% did not have them. Of all patients with impaired nervous regulation, 52.1% of patients had vegetoneurosis of the vagotonia type, 18.9% had symptoms of solaritis (solar syndrome), and 9.3% had signs of neurotic syndrome, often against the background of chronic arachnoiditis or post-traumatic encephalopathy. In 8.6% of individuals, there was a combination of vagotonia with solaritis or neurotic syndrome.
Comparison of the data obtained with the localization of the ulcer showed that in gastric ulcer the most common signs of solaritis, and duodenal ulcer - vagotonia. With the double localization of the ulcer, violations of the central nervous regulation and combined disorders in the nervous system were observed much more often.
In patients with high acid production of the stomach, vagotonia was detected in 94.1% of cases. In a hypoacid state, there was significantly more solaritis (44.2% of cases), combined disorders of nervous regulation (32.7% of cases) and disorders of the central nervous system (23.1% of cases). There were no signs of vagotonia in any case.
It should be noted that the number of patients with impaired nervous regulation increased depending on the severity of the disease.... So, with a mild course of the disease there were 83.2%, with an average severity of the disease - 92.9% and a severe course - 100%. At the same time, in the latter cases, the number of patients with concomitant disorders of nervous regulation significantly increased (with a mild course of the disease - 10.5%, with a severe course - 62.5%) and disorders in the central nervous system (6.0% and 25.0%, respectively. ).
It is also important that in patients in whom the disease proceeded with a clear seasonality of relapse, impaired nervous regulation was noted in 96.9% of cases, while without it - in 19.4%.
The question arises, what occurs due to disorders of nervous regulation and is the basis for the inclusion of pathogenetic reactions? Analysis of the available literature and our own studies show that disorders of nervous regulation lead to the emergence of inadequate reactions of the body to various stress factors affecting it. The manifestation of this is cholinergic and adrenergic shifts.
Nervous regulation disorders occurring during stressful situations, accompanied by cholinergic and adrenergic shifts, are the basis for inadequate action and interaction of various functional regulatory systems of the body, leading to a weakening of local and general defense mechanisms and the formation of pathogenetic reactions. In the course of treatment, the influence of etiological factors decreases, the nervous regulation is restored, the elimination of cholinergic and adrenergic shifts, which contributes to the normalization of the functioning of regulatory systems, the elimination of pathogenetic and the emergence of sanogenic reactions aimed at restoring defense mechanisms and eliminating the relapse of the disease.
Considering the above data on the morphogenesis of the ulcerative process, a large role in the pathogenesis of ulcer should be assigned microcirculation disorders in the mucous membrane of the gastroduodenal zone.
In the pathogenesis of ulcer, great importance is attached to dysfunction of the stomach... Traditionally, it is believed that one of the ulcer formation factors is acid-peptic, the action of which is due to an increase in the production of hydrochloric acid and pepsinogen with a simultaneous decrease in the production of protective mucus and alkaline-bicarbonate secretion by the glandular apparatus of the stomach. The activity of this factor in gastric ulcers is promoted by pylorospasm, stasis of food chyme, delayed evacuation, as well as duodenogastric reflux with regurgitation of bile acids and isolecithins, which weaken the protective mucous barrier. With duodenal ulcers, acidification of the pyloroduodenal environment may occur, associated with gastroduodenal dysmotility, a decrease in neutralization of the acidic contents of the stomach by the alkaline component of the duodenum.
An equally important functional system, the disruption of which affects the development and features of the course of ulcer, is pancreas. The association of stomach diseases with damage to the pancreas has long been noted by clinicians. It has been proven that pancreatic juice containing hydrocarbons neutralizes hydrochloric acid entering the duodenum, and its enzymes and hormones (alpha-amylase, lipase, trypsin, chymotrypsin, insulin, glucagon, somatostatin) not only contribute to the absorption and utilization of proteins carbohydrates, but also have a significant effect on the regulation of the secretory and motor functions of the stomach, the state of alkaline-acid balance and repair processes, including in the gastroduodenal zone.
After the works of Selye (1950, 1960), in which he reported that in animals under the influence of stress in the gastrointestinal tract ulcerations occur, accompanied by morphological and functional disorders of the adrenal cortex, they began to talk about big role pituitary - adrenal system in the pathogenesis of peptic ulcer disease. It is believed that an extraordinary increase in the glucocorticoid and mineralocorticoid function of the adrenal cortex contributes to the development of the ulcerous process. Glucocorticoids and mineralocorticoids during the period of action of etiological factors enhance microcirculatory disorders and necrotic processes, activates the acid-peptic factor.
An important role in the pathogenesis of ulcer is played by thyroid. A relationship was found between increased thyroid function and a number of clinical symptoms of relapse (irritability, emotional lability, weight loss, increased pulse pressure, sweating, distal hyperhidrosis, etc.), as well as with morphological changes in the gastroduodenal zone and gastric secretion.
Less explored is the question of the role systems parathyroid glands - C-cells of the thyroid gland in the pathogenesis of ulcer.
Clinical observations show that with hyperparathyroidism, ulcers are often found in the gastroduodenal zone. Parathyroidectomy leads to the elimination of gastric dyspepsia and ulceration syndrome.
It was found that parathyrin has an ulcerogenic effect on the mucous membrane of the gastroduodenal zone, and calcitonin has a protective effect.
The morphofunctional state of the gastroduodenal zone is influenced by another system - histamine and histamine-binding factors.
It is believed that the extreme hyperhistaminemia present in the acute phase of ulcer recurrence with a simultaneous decrease in the factors of inactivation of this amine is a pathogenetic reaction, one of the manifestations of the breakdown of adaptation mechanisms. At the same time, moderate hyperhistaminemia with activation of the histamine-binding properties of blood, observed in the subacute phase and, especially in the phase of scarring and epithelialization, is most likely of a sanogenic nature. and is due to the inclusion in this period of compensatory mechanisms aimed at eliminating the painful process.
Discussing the issues of the pathogenesis of ulcer, it is necessary to dwell on the state of the body's autoimmune reactions and their significance in ulcerogenesis. This is due to the fact that ulcer is a chronic recurrent disease characterized by periodic occurrence of inflammatory-necrotic processes in the gastroduodenal zone.
The affected tissue in the area of ulcers changes its individual biological identity so much that it acquires the properties of an antigen (autoantigen). This causes cellular infiltration in the area of altered tissue with the presence of macrophages and lymphocytes in it. The fact that immunocompetent cells are included in this reaction is evidenced by an increase in the blood of immunoglobulins, T- and B-lymphocytes. The predominant increase in T-lymphocytes may indicate the predominance of cellular immunity in this pathology, delayed-type reactions, and in particular autoimmune.
It follows from the above that pathogenesis and sanogenesis of ulcer are complex, interdependent processes, associated with an adequate or inadequate response of various functional systems of the body influencing the morphofunctional state of the gastroduodenal zone, the action of exogenous and endogenous ulcerous factors. The pronounced predominance of pathogenetic reactions over sanogenic ones determines the development or recurrence of the disease (scheme), and sanogenic over pathogenetic ones - its prevention or elimination. This point of view is confirmed by a dynamic study of the body's reactions in different phases of ulcer recurrence.
The acute phase of relapse occurs against the background of a pronounced effect of etiological factors and pathogenetic mechanisms.
The processes of ulcerogenosis are activated during this period of disruption of the activity of such functional blocks as the pituitary-adrenal and calcium-regulating systems, the thyroid and pancreas, and the liver.
Obviously pathogenetic reactions are an increased production of aldosterone, parathyroid hormone and thyroxine, a decrease in the secretion of amylase and bicarbonates by the pancreas, inadequate insulin secretion, as well as violations of the protein-forming and procoagulant functions of the liver, biliary dyskinesia.
During this period, immune disorders associated with hyperergic autoaggressive reactions to the ulcerous process can also form. It is not excluded that enhances inflammatory-necrotic changes and inhibits scarring of ulcers arising in the period of recurrence of the disease dysbacteriosis of the gastroduodenal zone.
Scheme ... The main pathogenetic mechanisms of peptic ulcer disease.
Etiological
impact
Decreased adaptive mechanisms. Changes in the nervous system and its regulation (trigger)
Adrenergic and cholinergic shifts, neurotrophic disorders
Dysfunction of the endocrine glands, especially the pituitary-adrenal system
Strengthening vasomotor reactions, the development of hypocoagulation, increased vascular wall permeability and tissue hydrophilicity. The emergence of microcirculatory disorders
Changes in the secretory and motor function of the stomach. Acid-peptic factor activation.
Strengthening immunological reactions, the formation of autoaggression. Increasing the formation of biologically active substances.
Development in the gastroduodenal region of areas of ischemia, plethora, hemorrhages, necrosis, erosions, ulcers
Excessive growth of mucosal microflora of the gastroduodenal zone
As the protective regime is observed and therapeutic measures are carried out, the activity of pathogenetic reactions begins to weaken and can become adequate to the painful process and the action of ulcerogenic factors, i.e. some of the pathogenetic reactions begin to acquire sanogenic properties, thereby strengthening the defense mechanisms. This is the reason for the transition of the disease to the subacute phase of relapse, and then to the phase of scarring and epithelialization (Fig.).
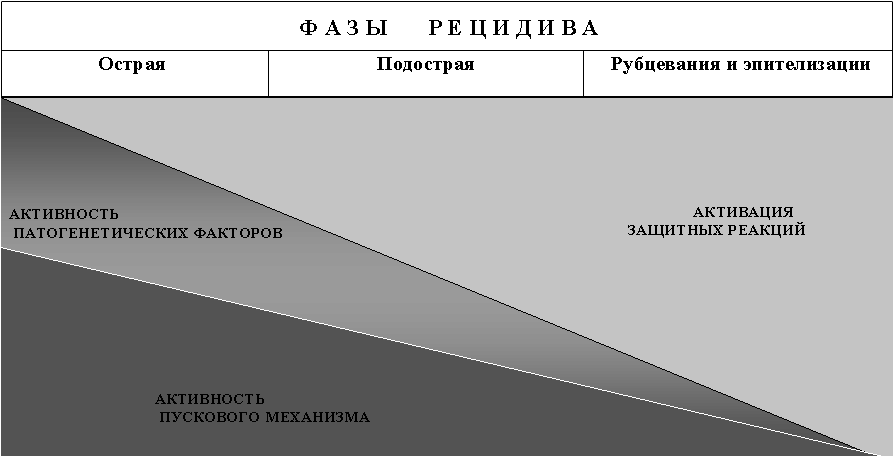
Rice. The activity of the trigger mechanism, pathogenetic and protective reactions in different phases of recurrence of ulcer
Subsequent possible relapses of the disease are associated with the repeated action of etiological factors leading to a violation of compensatory mechanisms and the formation of pathogenetic reactions.
However, it is necessary to know that the trigger mechanism, pathogenetic and sanogenetic reactions in individual patients may be different. These differences determine in each specific patient the peculiarities of the course of the disease, the localization of the ulcerative process, the state of the secretory and motor function of the stomach.
All of the above indicates that the activity of the ulcerous process, its features and clinical manifestations of the disease depend on the ratio and severity of the action of the trigger, pathogenetic and sanogenic reactions of the body. This means that when treating an exacerbation of the disease and carrying out anti-relapse measures, it is necessary not only to eliminate the influence of etiological factors, but also to suppress the activity of pathogenetic mechanisms and stimulate the body's defense reactions.
Classification of peptic ulcer. There is currently no generally accepted classification of YB.
According to the WHO international classification of the tenth revision (ICD-10, 1995) and the order of the Ministry of Health of the Russian Federation No. 125 dated 04/17/98, a stomach ulcer (stomach ulcer) is isolated - code K25, duodenal ulcer (PU) - code K26, peptic ulcer of unspecified localization - code K27, gastroduodenal ulcer, including peptic ulcer of the anastomosis of the stomach, leading and efferent loops of the small intestine - code K28. One should agree with the opinion of F.I. Komarov that this classification can be used for accounting and statistics purposes, but not in clinical practice.
We believe that the basis of the working classification of ulcer should be based on the localization of the ulcerous process, the features and severity of the course of the disease, the severity of relapse and complications. This classification principle gives the practitioner criteria for choosing a patient management tactics, resolving hospitalization issues, the duration of treatment and temporary disability, predicting possible complications of the disease, and determining the features of clinical examination.
We propose the following classification of nuclear weapons.
Since then, about 200 years ago, Cruvellier drew the attention of doctors to stomach ulcers, interest in this disease has been progressively increasing. Roughly the same applies to duodenal ulcer disease, which was described in detail much later (Moynihan, 1913).
Peptic ulcer disease is currently understood as a general, chronic, recurrent, cyclical disease, in which, as a result of a violation of the nervous and humoral mechanisms that regulate secretory processes, locomotor activity, blood supply and trophism in the gastroduodenal zone, in the stomach and duodenum, peptic ulcers are formed. Peptic ulcer disease is the most common disease of the digestive system. According to statistics, the frequency of its detection ranges from 8 to 12 cases per 1,000 adult population. This disease is much more common in men: so the ratio of duodenal ulcer among men and women is defined as 4: 1, and gastric ulcer - as 2: 1. It should be noted that ulcers in the duodenum are 3 times more common than in the stomach. As for the age of patients, the most common duodenal ulcer occurs in the age range from 25 to 50 years, and stomach - from 40 to 60 years.
ETIOLOGY
When studying the causes of the development of peptic ulcer disease, we will adhere to the point of view according to which the gastric and duodenal localization of the ulcer is considered in the context of one disease, which is based on almost the same etiological factors.
A conversation about any disease, including, of course, peptic ulcer, always begins with a consideration of the etiology and pathogenesis. In all known manuals, this section mainly covers only the pathogenesis of peptic ulcer disease, modestly passing over in silence the topic of etiology, the discussion about which first began (and has not yet ended) just a few years ago. As you probably already understood, we are talking about microorganisms called Helicobacter pilori, which the whole world has been talking about since 1983. They are curved gram-negative bacteria 3-4 microns long and 0.5-1.5 microns wide, having 4-5 thin flagella at one of the ends. Helicobacter pilori is found on the surface of the antral mucosa under the layer of integumentary mucus in almost 100% of patients with peptic ulcer disease. This microorganism is able to actively break down urea. food products with the help of the urease enzyme, which is accompanied by the formation of a cloud-like accumulation of ammonia around the bacterium, which protects it from the bactericidal action of hydrochloric acid of gastric juice. Based on the analysis and generalization of numerous observations on the pathogenic properties of Helicobacter pilori, C.S. Goodwin put forward a theory called the "leaking roof" concept, according to which Helicobacter pilori produces mucinase and lipase enzymes that break down protective gastric mucus. Thus, the integrity of the mucous gel is disrupted, which becomes less viscous and partly loses its protective properties, damage to microvilli, destruction of the cytoskeleton, intercellular connections occurs. When the protective layer of mucus is destroyed, the acid and pepsin of the gastric juice can cause erosion and ulceration of the epithelium.
Microbial contamination mainly affects areas with a high alkalizing function, which almost completely blocks the production of bicarbonates by the mucous membrane of the gastroduodenal zone.
Under the influence of a microorganism, reverse diffusion of hydrogen from the lumen of the stomach into the gastric glands may occur, as a consequence of this, the development of hyperchlorhydria and excessive release of histamine, which also contributes to ulceration. This mechanism is called the "proton funnel".
In addition, a correlation has been established between the content of Helicobacter pilori and the number of neutrophils in the gastric mucosa. These neutrophils are secreted in environment leukotrienes C4, which, under the influence of a microorganism, pass into more active D4, causing chronic vasospasm and hypoxia of the mucous membrane of the gastroduodenal zone.
In connection with important role played by Helicobacter pilori in the development of a peptic ulcer, there are many points of view trying to determine its place in this process. Some authors enthusiastically proclaim peptic ulcer infectious disease, others are more restrained, and tend to think about the mediated participation of the microorganism in its pathogenesis, through the development of type B gastritis and duodenitis. However, all are unanimous in one thing - Helicobacter pilori is an important, although not yet fully understood link, occupying one of the leading places in the onset and recurrence of peptic ulcer disease.
Now let's move on to consider other etiological factors underlying the consideration of peptic ulcer disease, adhering to the point of view according to which ulceration is a consequence of a violation of the interaction between the factors of acid-peptic aggression of gastric juice and the elements of protection of the mucous membrane of the gastroduodenal zone.
ALIMENTARY FACTORS They are the most ancient cause, with the help of which they tried to explain the development of peptic ulcer disease. In particular, factors such as long breaks between meals, large meals, hurried meals with poor chewing, dry food, etc. play a role.
So, rough, poorly chewed food can have a direct traumatic effect on the gastric mucosa, and with prolonged exposure, lead to the development of chronic gastritis. In addition, poor chewing of food entails insufficient wetting with saliva, which has buffering properties.
Significant breaks between meals lead to prolonged contact of hydrochloric acid, released during the interdigestive period, with the mucous membrane of the stomach.
Excessive food intake leads to overstretching of the walls of the antrum and, as a result, to an increase in the production of gastrin and hypersecretion of hydrochloric acid.
The nature of the diet also does not play last role... Various condiments and spices increase the secretion of hydrochloric acid and lead to desquamation of the epithelium.
HAZARDOUS HABITS Bad habits, which have a certain value in the occurrence of peptic ulcer disease, most often include such common household intoxications as smoking and alcohol abuse. In particular, smoking not only increases the risk of developing the disease, but contributes to its more severe course, significantly increasing the healing time of the ulcer. This is due to the fact that when tobacco smoke is inhaled, the secretion of hydrochloric acid is stimulated, due to the potentiation of the effect of histamine. In addition to this, the production of pepsinogen increases, there is a violation of the motility of the stomach and duodenum, which consists in a decrease in the tone of the pyloric sphincter and an increase in duodeno-gastric reflux of bile.
As for alcohol, the data on its effect on ulceration are not always unambiguous. However, there is no doubt about it Negative influence on the protective mucous barrier, it causes hyperemia of the gastric mucosa and duodenum, and in some cases ethanol can cause severe acute ulceration of the stomach. Long-term alcohol intake is accompanied by severe atrophic changes in the mucous membrane of the gastroduodenal zone with intestinal epithelial metaplasia. The effect of alcoholic beverages on secretion depends on the degree of strength, so high concentrations alcohol inhibits the production of hydrochloric acid, and weak alcoholic beverages promote the activation of acid secretion.
RECEPTION OF MEDICINAL PREPARATIONS is an important etiological factor in the development of peptic ulcer disease. This primarily applies to aspirin, indomethacin and corticosteroids. This is supported by statistical data, according to which taking acetylsalicylic acid 4 times a week increases the risk of ulcerogenesis by 3 times. Somewhat less often, peptic ulcer disease is caused by: anticoagulants, potassium chloride, derivatives of the nitrofuran series, ethacrynic acid, insulin, etc.
The mechanism of the damaging effect of drugs on the mucous membrane is very diverse, so reserpine and caffeine directly stimulate the secretion of hydrochloric acid; in corticosteroids, this effect is realized a second time, through hyperplasia of gastrin-producing cells of the stomach; non-steroidal anti-inflammatory drugs suppress mucus secretion and disrupt its qualitative composition, cause desquamation of epithelial cells, increase the degree of reverse diffusion of hydrogen into the mucous membrane, change the balance of prostaglandins, etc. Aspirin is especially dangerous, which causes a disorder of capillary circulation in the mucous membrane with the development of extensive hemorrhages and petechiae. Even a single intake of 2 aspirin tablets leads to the formation of petechial hemorrhages in the gastric mucosa, which persist for a day.
CONSTITUTIONAL AND HEREDITARY FACTORS N. D. Strazhesko (1927), after analyzing and revealing asthenic body type in 80% of peptic ulcer disease, concluded that "the patient is predisposed to peptic ulcer disease from birth due to his constitution." This assumption holds true only for patients with duodenal ulcers. In case of gastric ulcer, a reliable relationship between the constitutional type and the incidence rate was not revealed.
The importance of hereditary predisposition in the origin of peptic ulcer disease is difficult to overestimate. However, it should be noted that this statement mainly refers to duodenal localization. It is believed that hypersecretion of HCL and pepsin may be genetically determined. I would like to pay special attention to the predominant development of duodenal ulcer in persons with 0 (I) blood group, the gene of which is inherited in a recessive manner. It should be emphasized that for the manifestation of a hereditary predisposition, it is still necessary to influence the gastroduodenal zone of all the above etiopathogenetic factors.
NERVO-MENTAL FACTORS occupy one of the main places in the development of ulcer disease. This is due to the fact that in modern conditions there is a constant increase in the load on the human nervous system. A decline in living standards, a high mortality rate of children, premature death of relatives and friends, a premonition of insecure old age - all this creates the prerequisites for constant anxiety, grief, heavy emotional experiences, fear of the future and causes disruption of the functions of almost everyone in life. important organs and body systems.
The assumption about the influence of neuropsychic overstrain on ulcerogenesis was reflected in the cortico-visceral theory of the pathogenesis of peptic ulcer disease, formulated by K.M. Bykov and I.T. Curtsin, which in the 50s of our century became one of the main concepts of peptic ulcer disease.
According to the cortico-visceral theory, emotional overstrain leads to a violation of the functional state of the cerebral cortex. As a result, the inhibitory effect of the cortex on the subcortical centers (primarily hypothalamic) is weakened, where foci of "stagnant" excitement are formed, contributing to the occurrence of various endocrine and biochemical changes in the body, the development of disorders of the secretory and motor functions of the stomach and duodenum, vasospasm, disorder trophic processes in the mucous membrane, which ultimately leads to ulceration.
Abroad, a "stress" theory has been developed, according to which stressful situations, which include: negative emotions, hunger, cold, pain, immobilization, etc., lead to the emergence of protective reactions in the human body, which are realized through the pituitary-adrenal cortex system and passing through several stages in their development (anxiety, resistance, exhaustion). These reactions are of an adaptive nature and are an expression of the so-called "general adaptation syndrome". With excessive strength of stressful influences, a disruption of responses occurs, which can lead to the development of ulcerative lesions of the stomach and duodenum.
Currently, the psychoanalytic theory of "specific personality conflict" has become widespread. According to this concept, peptic ulcer disease is a consequence of a conflict that arose back in childhood... Boys and girls spoiled in childhood, becoming adults, retain an "unconscious desire" to remain in childhood conditions. This desire comes into conflict with the desire for independence and success that comes with growing up, which ends with the onset of peptic ulcer disease, and creates conditions for the chronicity of the disease.
VASCULAR FACTORS The mucous membrane of the stomach and duodenum does not have end vessels; they disintegrate into a network of arterioles and capillaries, anastomosed with each other at different levels. Arteriovenous shunts are located in the submucosa. It is possible that hypertonicity of the vagus nerve and hyperreactivity of the adrenal cortex can cause transient circulatory disorders in the shunt system. These changes contribute to the development of mucosal hypoxia, disrupt trophism and increase its vulnerability.
Now the question of the primacy of vascular disorders in the zone of the ulcer defect is widely discussed, a number of authors are inclined to assume that vascular damage in peptic ulcer disease belongs to the group allergic reactions of the third type, to the so-called immunocomplex pathology, and can be considered as local vasculitis, occurring with symptoms of endarteritis, the formation of immune complexes, tissue damage and subsequent scarring.
The pathogenesis of peptic ulcer disease is extremely complex and heterogeneous. Each theory taken in isolation is not able to explain all cases of the formation of a peptic ulcer and can only be considered as component v general concept pathogenesis, which is based on a violation of the interaction between the factors of acid-peptic aggression of gastric contents and the protective components of the mucous membrane of the gastroduodenal zone.
Under normal conditions, the aggressive properties of gastric contents are balanced by the high protective capabilities of the mucous membrane of the stomach and duodenum, reliably protecting it from self-digestion. An ulcerative defect can occur only when this equilibrium is disturbed either due to an increase in aggressive factors, or as a result of a weakening of the protective barrier. Moreover, with ulcers of different localization, the ratio of the factors of protection and aggression turns out to be ambiguous. If in the pathogenesis of duodenal ulcers the leading place is taken by an increase in the production of HCL and pepsin, then in the mechanisms of occurrence of gastric ulcers, the decisive role is played by the weakening of the protective properties of the mucous membrane.
AGGRESSIVE FACTORS In accordance with modern concepts, aggressive factors include, first of all, an increase in gastric acid and pepsin production, most often associated with irritation of the vagus nerve and hyperproduction of histamine and gastrin. Moreover, in most cases, there is a pattern according to which the closer the ulcerative defect is located to the pyloric section, the higher the acidity. Among the aggressive factors of ulceration, it is customary to consider disorders of gastroduodenal motility. First of all, these include the weakening of the tone and peristalsis of the stomach, which contributes: firstly, to the stretching of the walls of the antrum, which leads to an increase in the production of gastrin, and secondly, to the stagnation of acidic contents, which helps to lengthen the contact of hydrochloric acid with the gastric mucosa. (Theory of "antral stasis"). Another common theory considering the pathogenesis of peptic ulcer, based on disorders of gastroduodenal motility, is the theory of "duodenogastric reflux". The causes of reflux are associated with a violation of the tone of the pyloric sphincter and an increase in the peristalsis of the duodenum. The meaning of this theory is as follows: fatty acids and lysolecithin, when bile is thrown into the stomach as a result of duode-nogastric reflux, have a pronounced cytolytic effect on the mucous membrane, causing the destruction of lipid structures, degeneration of gastric mucus, the release of histamine and promoting an increase in the reverse diffusion of H + into the gastric mucosa. In addition, the content of thromboxane increases in the mucous membrane, causing local circulatory disorders. Finally, bile acids and pancreatic juice cause a persistent inflammatory response, leading to the development of antral gastritis with epithelial dysplasia.
SUPPRESSION OF PROTECTIVE FACTORS The high resistance of the gastric mucosa to unfavorable factors is ensured by the existence of a whole complex of protective factors: the production of gastric mucus, the secretion of bicarbonates, the rapid regeneration of the epithelium, and a sufficiently good blood supply. Violation of each of these mechanisms can serve as one of the pathogenetic links of ulcerogenesis.
GASTROMAL MUCIN (mucin) is a complex dynamic system colloidal solutions, which includes low molecular weight components that determine its structure (glycoproteins and mucopolysaccharides) electrolytes, leukocytes, bacteria, desquamated epithelium, secretory immunoglobulins, etc. The secretion of mucus occurs continuously and it represents the "first line of defense" of the gastric mucosa. The "second line" is the epithelial cells and the mucous membrane itself, it is assumed that there is also a third component of the protective barrier, which includes the intracellular mechanism of neutralization of H + (as discussed above).
Inhibition of the SECRETION OF BICARBONATES, which are contained in gastric juice and determine the alkaline component of secretion, is a prerequisite for the development of peptic ulcer disease. In accordance with modern concepts, on the surface of the mucus is dominated by acidic environment, and under the layer of mucus, between the mucus and epithelial cells, the medium is alkaline. This is a consequence of the release from the surface of epithelial cells into the submucous space, glycoproteins and bicarbonates to provide protection cell membranes... In addition to maintaining the pH gradient between the epithelial cells of the stomach and its lumen, bicarbonates are involved in the stabilization of the mucous gel and neutralize excess hydrochloric acid. Disorders of REGENERATION and TROPHIES of the gastric mucosa are important factor ulcerogenesis. Normally, the gastric mucosa belongs to the category of the most rapidly renewing cellular systems of the body. The regeneration of the epithelium is carried out every 4-6 days. With a peptic ulcer, this process can be delayed 3-4 times.
Reduced blood supply to the mucous membrane is an important pathogenetic factor of stress ulcers. The blood filling of the vessels of the mucous membrane decreases under the influence of alcohol, aspirin, histamine and corticosteroids. As a result of hypoxia, the normal ratio of the mucous-bicarbonate balance is disturbed, energy metabolism worsens, and the reverse diffusion of H + increases.
In addition to disrupting the normal balance between aggressive and protective factors of the gastroduodenal zone, humoral factors play a certain role in the pathogenesis of peptic ulcer disease. A direct correlation was noted between a decrease in the level of neurotransmitters (norepinephrine, dopamine) in the central nervous system, peripheral organs, an increase in the level of histamine in the stomach and the development of duodenal ulcers. Certain unanimity is expressed in relation to group E prostaglandins, which realize their antiulcer effect in two ways: the first is associated with intense suppression of gastric acid production; the second is determined by their cytoprotective capabilities and the ability to inhibit the activity of lysosomal hydrolases.
And, finally, concluding the conversation about the pathogenesis of peptic ulcer disease, it is necessary to touch upon the role of immune disorders in the development of the disease.
Great importance is attached to a sudden increase in the aggressive activity of neutrophils, which leads to their local accumulation, most likely in the zone of aseptic inflammation, most often caused by duodenogastric reflux. In the areas of accumulation, proteolytic enzymes begin to be released, creating an aggressive situation of a local nature. Mast cells in this area begin to degranulate with the release of histamine and serotonin, kinin factors are connected and a violent chain reaction with tissue destruction. Lysosomal enzymes, released during the destruction of macrophages, which phagocytose immune complexes, also take part in the occurrence of destruction. The mucous membrane is damaged from the inside, a zone of necrosis develops, which is then opened with the formation of an ulcer defect. The products of protein denaturation formed as a result of necrosis can take part in the formation of autoimmune reactions that contribute to the chronicity of peptic ulcer disease.
In some cases, food allergy is the cause of the development of ulcerative defects.
CLASSIFICATION
(P. Ya Grigoriev, E.P. Yakovenko, 1990)
1. Aggravation.
2. Phase of fading exacerbation (absence of clinical signs, fresh post-ulcer cicatricial changes, persistent inflammation of the mucous membrane).
3. The phase of remission (no clinical picture and no inflammatory changes in the mucous membrane). LOCALIZATION:
1. Stomach: cardiac section, subcardial section, fundic section, pyloric canal, lesser or greater curvature.
2. 12 duodenum:
A) bulb: front wall, back wall;
B) non-bulbous divisions. CLINICAL OPTIONS:
Newly diagnosed ulcer;
Large ulcer;
Giant ulcer (more than 30 mm in diameter in the stomach and 20 mm in the duodenum 12);
Callous ulcer (an ulcer with dense edges and bottom due to the intensity of the development of scar tissue);
Scarring ulcer (in case of a decrease in size and depth);
Chronic ulcer (in the absence of signs of scarring within 30 days);
"kissing" ulcers;
Fresh, re-emerging ulcer (the appearance of an ulcer in another part of the stomach or duodenum 12 relative to the previous inflammation). STATE OF ESOPHAGOGASTRODUODE-NAL MUCOSA: active type B gastritis, mixed gastritis, atrophic gastritis, erosive gastritis, duodenitis, gastroduodenitis, pylorobulbitis, erosive gastroduodenitis, erosive pylorobulbitis, esophagitis, erosive. BY ACID PRODUCTION FUNCTION OF THE STOMACH: normal acidity; increased acidity; reduced acidity; true achlorhydria. COMPLICATIONS: bleeding, bleeding and acute post-hemorrhagic anemia, bleeding and chronic post-hemorrhagic anemia, perforation, penetration, stenosis, malignization, perivisceritis, cicatricial deformity.
CLINICAL PICTURE
COMPLAINTS The leading symptom in the clinical picture of peptic ulcer disease is pain; in its absence, the disease is usually not diagnosed. It is known that the mucous membrane of the gastrointestinal tract does not have sensitive innervation, therefore, pathological processes (inflammation, erosion, etc.), as well as therapeutic effects (biopsy, diathermocoagulation) without secretory-motor disorders of the organ do not cause pain. When the pathological process spreads to the muscular and serous membranes of the organ and disorders leading to increased pressure and stretching of the walls of the stomach and duodenum, pain occurs, called visceral. By its nature, it is dull, of moderate intensity, spilled, periodic. If the parietal sheet of the peritoneum, which has sensitive spinal innervation, is involved in the pathological process, then somatic pain occurs, which is perceived as sharp, acute and limited.
Pain in peptic ulcer disease can be of a different nature: aching, dull, burning, cramping or boring. They, as a rule, are of an increasing nature, forcing patients to take a forced position: on the stomach, on the side, with their knees pulled up to the stomach.
The duration of pain is most often 1-3 hours, less often they last from 30 minutes to an hour, very rarely there are short-term pains lasting less than 30 minutes.
In order to relieve pain, patients resort to the use of alkalizing and acidity neutralizing drugs, I.P. Pavlov at one time compared the effect of such drugs (especially in case of duodenal ulcer) with the effect of nitroglycerin in angina pectoris.
The localization of pain in peptic ulcer disease is different and, unfortunately, is not always determined by the location of the ulcer defect. However, most often, when an ulcer is localized on the lesser curvature of the stomach, pain occurs in the left side of the epigastric region, with ulcers of the cardiac part of the stomach - behind the xiphoid process, when localized in the duodenum - in the epigastric region to the right of the midline, 5-7 cm above the navel.
A specific place in the diagnosis is the irradiation of pain. In case of gastric ulcer, irradiation to the left half of the chest, the left scapula and the xiphoid process is possible, which can lead to an incorrect diagnosis of ischemic heart disease. In patients with duodenal ulcer localization, the most common area of irradiation is the lumbar region.
In accordance with the classical and clinical canons, gastric ulcer and duodenal ulcer are characterized by pain arising in different phases of the digestive period. It is generally accepted that early pain that occurs 0.5 - 1 hour after eating is characteristic of ulcers of the middle and lower third of the stomach. With the localization of the process in the cardiac department and the upper third of the stomach, pain may appear immediately after a meal.
Late pain that occurs 2-3 hours after eating is regarded as a characteristic sign of duodenal ulcer disease. With this localization, there are often "hungry" pains that appear 6-7 hours after eating and stop after taking a small amount of food (crackers, cookies, several sips of water). Nocturnal pains are most often disturbed between 11 pm and 3 am and are considered the equivalent of "hungry" pains. It should be noted that for the duodenal localization of the ulcer, seasonal exacerbations are more characteristic than for the gastric one.
With combined gastroduodenal ulcers, a combination of several pain syndromes (for example, early, late and nocturnal) is possible. This pattern of pain occurrence is most often explained by the level of secretion of hydrochloric acid, its binding by buffer components of food and the nature of the evacuation of gastric contents.
Unfortunately, in practice, such a strict rhythm of the onset of pain syndrome, and most importantly, a clear connection between the time of onset of pain and the localization of the defect in the gastroduodenal zone is not always found. This is due to the early use and long courses of treatment with highly effective antiulcer drugs and some change in the clinical picture of the disease in modern conditions.
In addition to the pain syndrome of patients with peptic ulcer disease during an exacerbation, various dyspeptic disorders are often disturbed, which are based on a violation of the evacuation of stomach contents due to prolonged spasm and severe inflammatory edema of the pylorus and duodenal bulb.
Nausea - is not a pathognomonic symptom only for peptic ulcer disease (it can occur with gastritis, chronic pancreatitis, chronic cholecystitis). Most often found in duodenal ulcer and combined gastroduodenal ulcers. More typical for women.
VOMITING - occurs mainly with gastric ulcer localization and in most cases is associated with an increase in the tone of the vagus nerve. It occurs during the period when the stomach is freed from the last food debris and is apparently caused by irritation of the hyperkinetic stomach with gastric juice. Vomiting with exacerbation of peptic ulcer disease appears without prior nausea, usually at the height of the pain syndrome and brings immediate relief, and therefore patients often use artificially induced vomiting to eliminate pain.
It should be noted that with stomach ulcers, vomiting occurs immediately or after 1-1.5 hours after eating, and with duodenal ulcer - after 2-2.5 hours.
Heartburn (burning sensation in the epigastric region and behind the sternum) is more characteristic of peptic ulcer disease with duodenal localization. It is somewhat more common in males. Heartburn may precede the onset of pain, be combined with them, repeating the circadian rhythm of the pain syndrome, or persist after the disappearance of other symptoms of exacerbation of peptic ulcer disease.
The occurrence of heartburn is most often associated with two reasons: most often it is caused by reflux esophagitis, i.e. peptic action of gastric contents on the esophageal mucosa and mechanical stretching of the esophageal walls as a result of gastroesophageal reflux. As a second reason, I would like to note the hypersecretion of hydrochloric acid, which causes irritation of the mucous membrane of the gastroduodenal zone.
Belching - occurs quite often with stomach ulcers and is often combined with regurgitation and salivation. In the mechanism of belching, concomitant hernia of the esophageal opening of the diaphragm, cardia insufficiency and reflux esophagitis may be important. The most characteristic eructation is sour, in the presence of duodeno-gastric reflux, eructation of bitterness and bile appears, and with the development of cicatricial ulcerative stenosis of the pylorus, an eructation with a smell rotten eggs... Frequent, loud belching with air, caused by swallowing air, aerophagia, is not characteristic of peptic ulcer disease and only in some cases is combined with it. Appetite in most patients remains good. Decreased appetite is rare enough and in uncomplicated ulcers it never reaches the degree of aversion to food. It is necessary to point out a sometimes occurring condition called sitophobia (fear of eating due to the possible occurrence of pain).
In some patients, there is a significant increase in appetite, especially with duodenal ulcers, there is a "painful feeling of hunger".
In some patients, increased salivation (hypersalivation) periodically appears. This usually occurs in the form of isolated short-term attacks preceded by nausea and autonomic disorders are the most common cause. In patients with peptic ulcer disease, various bowel dysfunctions are often encountered. To the greatest extent, this is inherent in duodenal ulcers. Most often, constipation occurs, they are based on: an increase in the tone of the vagus nerve, a kind of diet devoid of fiber, in-bed regimen. It should be emphasized that the occurrence of constipation coincides with the phase of exacerbation of peptic ulcer disease, and during the period of remission they may disappear.
Much less often with ulcerative lesions of the stomach, diarrhea occurs, associated with a violation of the processes of digestion and absorption, concomitant pancreatitis and avitaminosis.
Having characterized the main complaints of patients with peptic ulcer disease, one should once again emphasize the complexity of their correct interpretation. On the severity of clinical manifestations of the disease big influence have such factors as: gender, age, localization of the ulcer, its size, etc., which will be considered a little later.
GENERAL INSPECTION With a general inspection, you can get whole line characteristic features, although it should be noted that their diagnostic value is currently not as great as before.
For peptic ulcer of the duodenal ulcer, an asthenic type of physique is characteristic, with gastric ulcer such a pattern is less common.
The pallor of the skin revealed in some patients may indicate the presence of obvious or latent bleeding. With a normal content of hemoglobin and erythrocytes, pallor may be due to spasm of small arterioles, which occurs against the background of severe pain syndrome.
When examining the oral cavity in patients, you can often find carious teeth, less often periodontal disease is detected. These factors can disrupt the mechanical processing of food and contribute to the development of chronic stomach diseases. When examining the tongue, during an exacerbation, it is noted white bloom, which is associated with the presence of chronic gastritis. Quite often, it is possible to detect different areas of desquamation of the epithelium not correct shape... In cases of atrophic gastritis with a reduced secretory function, the papillae are smoothed. When the ulcer is localized in the duodenal zone, hypertrophy of the filiform and mushroom papillae of the tongue is observed. In cases of accession complications, such as perforation and penetration, the tongue becomes dry and thickly coated.
Important data for the diagnosis of peptic ulcer disease is provided by methodically correct palpation of the abdomen. You should not limit yourself to palpation of the abdomen only in the horizontal position of the patient, the subcardial region and the lesser curvature are better palpated in the standing position.
With superficial (approximate palpation), especially during an exacerbation of peptic ulcer disease, local pain in the epigastric region is often determined, and with localization of an ulcer in the stomach, this zone is located to the left of the midline, and with duodenum ulcers - to the right. With the defeat of the cardiac part of the stomach, soreness is located directly at the xiphoid process.
In almost half of the patients, with superficial palpation, it is possible to determine the local tension of the muscles of the anterior abdominal wall (muscle defense). This symptom is a reflection of the involvement of the peritoneal lining in the process, from where, along the pathways of viscero-motor reflexes, irritation is transmitted to the abdominal muscles. In the vast majority of patients, muscle rigidity is determined in the right half of the epigastric region. Being associated with a clinical exacerbation of the disease, muscle tension is relatively unstable, it weakens very quickly and completely disappears with an improvement in well-being. Generalized tension of the muscles of the anterior abdominal wall is not typical for uncomplicated peptic ulcer disease.
Deep methodical palpation sometimes allows, in emaciated subjects, to the right of the midline, 3-4 cm above the navel, to determine a painful, spasmodic and rumbling pylorus, palpable in the form of an elastic band. In very rare cases, it is possible to palpate the ulcer itself, more precisely, the inflammatory edema near the callous ulcer. With the formation of cicatricial-ulcerative stenosis and with a sharp hypersecretion of gastric juice, it is possible to determine the positive symptom of Vasilenko - a feeling of "splash noise" with jerky pressure in the epigastric region, 7-8 hours after a meal.
Percussion tenderness is considered a more valuable diagnostic criterion than palpation. In this regard, the symptom of MENDEL is very characteristic of the exacerbation of peptic ulcer disease, which is the definition of a zone of local pain during percussion in the epigastric region. The size of such a zone is different - from the size of the cherry to the size walnut, most often it has a somewhat elongated or oval shape and is located in the right half of the epigastric region.
In addition to the local symptoms revealed in the study of the abdominal cavity in peptic ulcer disease, rather characteristic changes are almost always observed on the part of other organs and systems.
On the part of the cardiovascular system in patients with peptic ulcer disease, there is often a tendency to hypotension, bradycardia and a decrease in cardiac output, which is associated with an increase in the tone of the vagus nerve and a decrease in the mineral-corticoid activity of the adrenal glands. It should be noted that the above changes are more characteristic of duodenal ulcers and mainly in young patients.
When examining patients with peptic ulcer certain attention should be given to the state of the respiratory system, since chronic nonspecific lung diseases are often found in this disease. Moreover, these combinations are more characteristic of stomach ulcers, which, apparently, is due to the older age of this category of patients, the predominance of males and a large percentage of smokers.
Certain changes relate to changes in the functional state of the nervous system. In this category of patients, various autonomic disorders occur: first of all, it is increased sweating, changes in dermographism, a feeling of heat or cold, tremor of hands, etc. Complaints of general weakness, fatigue, asthenia, headaches, poor sleep, irritability, and unstable mood are frequent. All this dictates the necessity of prescribing consultations of a psychotherapist for such patients and the introduction of tranquilizers, sedatives and antidepressants into the treatment regimen.
LABORATORY DATA
A clinical blood test can provide a lot of information to clarify the diagnosis of peptic ulcer disease. With the localization of the ulcer in the duodenum, some patients may experience erythrocytosis and an increase in the level of hemoglobin. One of the hypotheses explaining erythremia associates irritation of the mucous membrane of the duodenum and the pyloric part of the stomach with the stimulation of the secretion of an internal antianemic factor in the fundic part of the stomach. In patients with gastralgic localization of the ulcer, there is a tendency to moderate hypochromic anemia, which is most often associated with the presence of latent gastrointestinal bleeding or is one of the early signs malignancy.
The number of leukocytes, in most cases, remains normal. Moderate leukocytosis can occur after bleeding, a significant increase in the number of leukocytes and neutrophilic shift indicate the presence of complications (perforation or penetration of the ulcer).
ESR in uncomplicated ulcers is within the normal range or slightly reduced; as the reasons for the development of this phenomenon, erythrocytosis, dysproteinemia and lability of the autonomic part of the nervous system are most often noted. An increase in ESR indicates the presence of anemia, bleeding or malignancy of the ulcer.
Urinalysis has no characteristic features with this disease, however, it must be borne in mind that peptic ulcer disease is often combined with urolithiasis and other diseases of the urinary system.
General analysis feces remains normal only in half of the patients, due to concomitant pathology from the biliary tract, pancreas and intestines, an increase in fiber content, creatorrhea, steatorrhea, amilorrhea is found during scatological studies.
Fecal occult blood analysis should be performed in all patients with exacerbation of peptic ulcer disease. Gregersen's benzidine reaction is very sensitive and becomes positive with blood loss exceeding 2 ml, and normally up to 1 ml can be lost with feces. However, this reaction is not very specific, since it can be positive for bleeding gums, pharyngeal and nosebleeds, helminthiasis, hemorrhoids, erosive gastroduodenitis, intestinal polyposis, blood diseases, etc.
ADDITIONAL RESEARCH METHODS play an extremely important role in the diagnosis of peptic ulcer disease, back in the 80s there was a point of view according to which the diagnosis of this disease should in no way be based on the patient's complaints and that it can only be made on the basis of radiological and endoscopic data. However, as you understand, this is an overly categorical and polar point of view that runs counter to our ideas about the priority of clinical data in the diagnosis of any nosological form.
The most common, very safe, affordable and objective is the X-ray method of research, which, in addition to morphological changes in the gastroduodenal zone, gives an idea of the functional changes in the organs under study. Using this research method, it is almost always possible to confirm pyloric stenosis, gastric emptying disorders, diverticulosis, but ulcerative defects are detected in 75-80% of cases, erosive changes are practically not visualized.
The main X-ray sign, which makes it possible to diagnose an ulcer with confidence, is the "niche" symptom. An ulcer niche is a structureless depot of barium mass, usually of a regular shape, with clear contours. Around it, upon careful examination, a rim of enlightenment is visible - an inflammatory shaft, to which the folds of the mucous membrane converge. It should be emphasized that bleeding ulcers are rarely detected, their crater is filled with thrombotic masses, and the inflammatory shaft is sharply reduced, which makes them X-ray negative. Large ulcers from 0.5 to 2-3 cm are most easily recognized.
As auxiliary diagnostic criteria, it should be noted: increased motility, hypersecretion, local spasm, deformation of the organ wall, accelerated evacuation of barium suspension, reflux, etc.
Esophagogastroduodenoscopy, carried out using a flexible endofibroscope, is the most reliable method for diagnosing peptic ulcer disease. With the help of this research method, it is possible not only to identify an ulcer defect, to ensure control over its scarring, but also to conduct a targeted biopsy, which makes it possible to assess the nature of changes in the mucous membrane and guarantees the accuracy of the diagnosis.
The endoscopic picture of an exacerbation of the ulcerative process in most cases is determined by an ulcerative defect and inflammation of the mucous membrane. Ulcers vary in size and shape, but most often they are round. The edges are high, even, clearly outlined, the slopes of the ulcer crater are steep, the bottom is covered with a whitish or yellowish-gray bloom. The mucous membrane around the ulcer is inflamed, this is manifested in its swelling, hyperemia, it looks like a raised roller surrounded by a zone of bright hyperemia.
In a biopsy from the bottom and edges of the ulcer, detritus, decaying leukocytes, erythrocytes and desquamated epithelial cells are found. In the periulcerous zone - a picture of acute inflammation with edema and significant vascular congestion. The infiltrate is dominated by eosinophils, neutrophils, lymphocytes, plasma and mast cells.
An ulcer in the healing stage is characterized by a decrease in periulcerous inflammation, it takes a slit-like shape, the inflammatory shaft and perifocal hyperemia decrease or disappear.
A post-ulcer scar appears at the site of a fresh ulcer in the form of a more hyperemic pink section of the mucosa with a stellate or linear retraction of the wall. Over time, the "pink scar" stage is replaced by the "white scar" stage, this occurs after the transformation of granulation tissue into fibrous connective tissue.
The study of gastric secretion should be carried out for each patient with peptic ulcer disease. The main indicators of gastric secretion include:
1) the volume of gastric juice;
2) acid composition of the content;
3) the flow rate of hydrochloric acid and pepsin.
1. Determination of the volume of gastric juice is important in assessing the hourly tension of secretion and evacuation-motor disorders of the stomach and duodenum.
2. The acid composition of gastric contents is usually determined by: - the total acidity of gastric juice, indicating the number of functioning parietal cells; - bound hydrochloric acid - reflecting the content of mucus and protein substances in the gastric juice with buffering properties; - free hydrochloric acid is an active part of hydrochloric acid dissociated into H + ions, which is capable of damaging the mucous membrane of the gastro-duodenal zone.
3. The flow rate of gastric juice per unit of time is calculated using special formulas, which you will get acquainted with in practical training. When it comes to peptic ulcer disease, it must be borne in mind that it is a chronic disease with a wave-like course, expressed by periodic seasonal exacerbations and remissions of varying duration.
The above clinical picture, laboratory data and data of additional examination methods are characteristic of the phase of exacerbation of the disease, in which, along with active inflammation in the pyloroduodenal zone, in most cases there is an ulcerative defect. However, it should be noted that a relapse of ulcerative damage is not always observed with an exacerbation. These two concepts should be clearly distinguished: exacerbation is the clinical and morphological manifestations of the disease, reflecting its chronic nature, and their dynamics; relapse - a defect of the mucous membrane that appears in most cases at the height of exacerbation.
The phase of fading exacerbation occurs when the ulcerative defect has already healed (stage of "pink scar"), there is no characteristic clinical picture, but there is a pronounced inflammation in the mucous membrane of the stomach or duodenum. This phase begins at different times from the start of treatment. The average time for scarring of ulcers in the cardiac section is from 30 to 60 days, in the body of the stomach from 40 to 75 days, in the pyloroantral section of the stomach - from 50 to 100 days.
The phase of remission, when, along with the healing of the ulcer defect, there is a complete relief or a significant decrease in the activity of inflammatory manifestations.
Consequently, the division of peptic ulcer into phases is based on the inflammatory process, which is the only indicator that determines the recurrent course of the disease. An ulcer occurs only at the height of inflammation, and its full-fledged scarring is possible only after the latter is reduced, and the localization of inflammation almost always determines the localization of the ulcer.
Thus, if there is an indication of a peptic ulcer in the anamnesis, and only high activity is found during endoscopic examination inflammatory process in the mucous membrane of the gastroduodenal zone, accompanied by a typical clinical picture, the diagnosis of peptic ulcer in the acute phase should be considered justified, despite the absence of a defect. Now it is necessary to briefly dwell on the features of the clinical course of peptic ulcer disease, depending on the localization of the ulcerative process. We discussed in detail the clinical manifestations of gastric ulcer and duodenal ulcer. Now it is necessary to stipulate those differences that are characteristic of a narrower and more detailed localization of ulcers in different parts of the pyloroduodenal zone.
Ulcers of the cardiac part of the stomach are characterized by an unusual pain syndrome, which is localized most often in the upper part of the epigastric region, behind the xiphoid process, sometimes behind the sternum, this often does not fit into the description of the classic forms of the disease and can proceed under the mask of angina pectoris, cholecystitis, or left-sided pleurisy. Pain syndrome occurs, as a rule, during or immediately after eating. Very often, ulcers of such localization are accompanied by chronic atrophic or subatrophic gastritis with reduced acid-forming function of the stomach. Despite the fact that ulcerative defects of the cardiac part of the stomach are larger than ulcers of other localization, they are diagnosed less often and even with endoscopic examination are not always detected, quite often they are complicated by bleeding and malignant.
Pyloric canal ulcers are more common in young men in 5% of cases. They are accompanied by persistent, strong, poorly controlled late and hungry pains localized in the right half of the epigastric region and typical irradiation to the back or upper lumbar region. Nausea, vomiting, and heartburn are very common. In terms of size, these ulcers are always small and in half of the cases are not diagnosed by X-ray examination. The acidity of the gastric juice, as a rule, is increased.
Extra-bulbous ulcers most often occur with a clinical picture characteristic of duodenal ulcer. However, they are often accompanied by symptoms resembling cholecystitis, pancreatitis and enterocolitis. Pain syndrome is localized in the upper right quadrant of the abdomen or in the back with downward radiation. A very typical complication is recurrent bleeding, accompanied by melena, dizziness, dry mouth and other symptoms of post-hemorrhagic anemia. Sometimes exacerbation of extra-bulbous ulcers is accompanied by jaundice due to the spread of the inflammatory process to the sphincter of Oddi.
Peculiarities of the course of peptic ulcer disease in young people primarily relate to the localization of the lesion, which, as a rule, is located in the distal parts of the stomach. A distinctive feature is an acute, sudden onset, often manifested by gastrointestinal bleeding or ulcer perforation. The characteristic and localization of pain syndrome in young people is identical to middle-aged patients. The appetite is always preserved. Acidity at the same localization turned out to be higher in young people. The size of the ulcer defect in persons younger age turned out to be less than in other age groups. There is a direct correlation between the age of patients and the rate of ulcer scarring.
Peculiarities of the clinic of peptic ulcer disease in persons of older age groups. Exacerbation of the disease in elderly and senile people is not seasonal; pain, as a rule, is not associated with food intake; the disease proceeds against the background of reduced gastric acid secretion and is characterized by a tendency to slow healing of the ulcer. Often in the elderly, ulcers are formed not as a consequence of peptic ulcer disease, but as a result of atherosclerotic lesions of the mucous membrane of the gastroduodenal zone.
DIFFERENTIAL DIAGNOSTICS
Should be performed primarily with malignant neoplasms of the stomach. It is reasonable to talk about two possible variants of malignant ulceration. The first is the malignancy of a benign stomach ulcer; to the second - infiltrative-ulcerative or primary ulcerative form of stomach cancer (cancer-ulcer). Sometimes these two forms can be combined. Given the oncological alertness, peptic ulcer disease should be considered as a precancerous condition.
In favor of malignancy, first of all, a long history of peptic ulcer disease, a change in the usual clinical picture: the loss of the connection between the occurrence of pain with food intake, the appearance of a permanent pain syndrome, the occurrence of anemia, accelerated ESR, weight loss, a sharply positive reaction of feces to occult blood. The final conclusion about the presence of ulcer malignancy can only be made after histological examination. Typical signs are: the penetration of the ulcer into the muscular layer of the stomach, the presence of pronounced fibrosis and obliterating endarteritis at the bottom of the ulcer, localization of the carcinoma focus in the edge of the benign ulcer.
With an ulcerated form of cancer average age patients is 65 years old. The localization of the ulcer in the area of the greater curvature of the stomach should always be alarming. As a rule, ulceration in this form of cancer is much larger than that of a common ulcer and can be 2-3 cm in diameter. Distinctive feature is a short (less than one year) "ulcerative history". The onset of the disease can be acute and manifest as gastrointestinal bleeding, or gradual with the onset of moderate persistent pain and dyspeptic symptoms with a predominance of vomiting. When studying the acidity of gastric juice, achlorhydria is very often observed. X-ray examination plays a decisive role. Finding a "niche" irregular shape and uneven edges, revealing the breakage of the folds of the mucous membrane and the rigidity of the stomach wall at the site of ulceration, always makes it possible to suspect a neoplasm and conduct an endoscopic examination.
TREATMENT
Conservative treatment of patients with peptic ulcer disease must necessarily be complex, i.e. include not only the appointment of medicinal antiulcer drugs, but also a wide range various events: dietary nutrition, cessation of smoking and alcohol intake, normalization of work and rest, spa treatment, etc.
This whole complex is designed to perform two tasks: to provide treatment for relapse and to contribute to the lengthening of remission (preventive treatment).
The criterion for the effectiveness of the therapy is:
Disappearance of clinical manifestations;
The presence of a healed ulcer (according to fibrogastroscopy);
No signs of mucosal inflammation.
Relapse should be treated in a hospital setting. - Health food still remains an integral part of the complex therapy of peptic ulcer disease, although many of its principles are currently being challenged and revised. Patients should be advised frequent (5-6 times a day) and fractional meals, after eating, they should rest for 15 minutes. Compliance with the rhythm of food intake provides a long-term averaging of gastric contents and continuous, translational motion food chyme along the digestive tract, which helps to eliminate regurgitation syndromes. The principle of thermal, mechanical and chemical sparing of the gastric mucosa retains its validity.
In the phase of a sharp exacerbation of peptic ulcer disease, diet N 1a is prescribed, for a period of 2-3 days. These are dishes boiled or steam, liquid or puree-like consistency. Patients are allowed mucous broths of cereals (oat, rice, semolina), soufflé or mashed fish and meat, soft-boiled eggs, jelly, milk, cream.
Diet No. 1b includes crackers, bran decoctions, cereals, mashed with milk, mashed cheese, creamy, olive and sunflower oil... It should be remembered that the above diets are of more historical interest, since they are not complete, do not bring satisfaction to the patient and, therefore, should not be prescribed for a period of more than 5-6 days.
The most physiological and moderately sparing diet is diet number 1, which provides for restriction table salt(up to 8-10 g) and includes white stale bread, dry biscuits, sou-pies from mashed cereals, vegetables, dairy products pasta, beef, veal, chicken, turkey, rabbit meat, lean fish, vegetable purees (potatoes, zucchini, carrots), steam omelet, cream, cottage cheese, sour cream, cheese mass. This diet is prescribed for the entire period of exacerbation, including the phase of fading exacerbation.
It is extremely important to carry out sanitation of the oral cavity and prosthetics of missing teeth, which affects the natural machining food. - Drug therapy of peptic ulcer in recent times has been enriched with a number of highly effective drugs, therefore, paying tribute to the classic treatment regimens, we will dwell in more detail on new groups of drugs and modern approaches to the treatment of this disease.
As you know, the therapy of any disease can be considered effective only if it is based on the pathogenetic principle. The pathogenesis of peptic ulcer disease is extremely complex, not fully understood, including many different links.
The classification of antiulcer drugs is largely arbitrary, since a number of drugs act simultaneously on various links in the pathogenesis of the disease. But nevertheless, the following groups are distinguished:
ANTISECRETARY DRUGS
1. Antacids, adsorbents and astringents are one of the oldest and most numerous groups of drugs, they neutralize hydrochloric acid in the stomach, without affecting its production, and reduce the activity of pepsin. When these drugs are taken, molecules are formed in the stomach cavity with the neutralization of hydrochloric acid carbon dioxide, water and the corresponding metal salts.
The main representatives of this group are compounds of alkaline and alkaline earth metals: sodium bicarbonate, magnesium and calcium carbonates, magnesium oxide and trisilicate, aluminum hydroxide, etc. Bismuth preparations have not so much a weak neutralizing effect as an astringent and adsorbing effect.
According to the speed of action, the drugs are divided into: - quickly absorbed (action time 10-20 minutes): soda, sodium bicarbonate, magnesium oxide; - non-absorbable (long-acting drugs): aluminum hydroxide, magnesium trisilicate.
Often, all of the above antacids are part of combined drugs, such as: almagel, phosphalgel, gluse-varnish, tepilta, compensated, sucralfat, megalac, vikalin, vika-ir.
Despite the fact that all drugs neutralize hydrochloric acid, each of them has certain characteristics. In particular: - almost all normalize the motor function of the stomach and duodenum due to more quick opening the gatekeeper and expulsion of the "averaged" gastric contents into the intestinal cavity; - they have a cytoprotective effect in different ways: they stimulate the production of prostaglandins, have an astringent and enveloping effect (magnesium trisilicate and bismuth preparations), adsorb bile acids (aluminum preparations) - inactivate the action of pepsin by absorption (aluminum, bismuth); - have a positive effect on local hemostasis.
Antacids are prescribed one hour after meals and at bedtime.
Among side effects I would like to note, first of all, a secondary (after the initial antacid action) increase in the secretion of hydrochloric acid. A serious complication is the development of "lactic-alkaline syndrome" with the combined use of antacids and milk (thirst, decreased appetite, polyuria), more rarely occurs urolithiasis disease, tooth decay. 2. Preparations with a receptor pathway for the correction of disturbances in the secretion of hydrochloric acid.
2.1. Anticholinergics - block the interaction of acetylcholine with chlinoreceptors and thereby weaken or completely stop normal and pathological impulses from the central nerve formations to the periphery and vice versa. Anticholinergics reduce acid production mainly by reducing the volume of secretion, inhibit the release of gastrin and pepsin, and reduce the motor activity of the stomach and duodenum. All drugs in this group should be prescribed taking into account the rhythm of the onset of pain. Due to the fact that the maximum of their action is reached after 2 hours, for early pains should be taken 1-1.5 hours before meals, and for late and hungry pains 1 hour after meals.
There are NON-SELECTIVE M-anticholinergics, which, to a greater or lesser extent, have side effects: dry mouth, disorder of accommodation, tachycardia, difficulty urinating, constipation, insomnia, dizziness. The most commonly used are:
Atropine (s / c 0.5-1 ml of 0.1% solution, 2-3 times a day until dry mouth appears), metacin (i / m 1 ml of 0.1% solution, 2 times per day or by mouth 0.002-0.005 g 3 times a day), platifillin (i / m 1-2 ml 0.2% solution 2 times a day), pro-bantin (1 tablet (15 mg) 3 times per day), chlorosyl (i / m 1 ml of 0.1% solution, 2 times a day). At present, the drugs of this group have lost their former attractiveness and are of certain interest more from a historical point of view.
After establishing the heterogeneity of muscarinic receptors, CE-LECTIVE M-anticholinergics were synthesized, which include a relatively new and superior to its predecessors in terms of effectiveness, the drug gastrocepin. It significantly inhibits the production of pepsin and hydrochloric acid, dilates the vessels of the gastric mucosa, prevents the development of gastroesophageal reflux and increases the amount of mucus in the interdigestive period. As a rule, there are no side effects when prescribing medium doses. Ga-strocepin is usually prescribed 50 mg (2 tablets) 2 times a day (morning and evening). 2.2. Histamine H2 receptor blockers
This relatively a new group medicines, without which it is difficult to imagine a successful treatment of peptic ulcer today. It is no exaggeration to say that blockers of histamine receptors are the most common antiulcer drugs abroad.
The stimulating effect of histamine on gastric secretion is carried out through the H2 receptors of the parietal cells of the stomach. Drugs that block these receptors have a pronounced antisecretory effect. In therapeutic doses, they reduce the basal gastric secretion of hydrochloric acid, inhibit the production of pepsin, reduce nocturnal acid secretion, do not affect the motor activity of the stomach, increase the synthesis of prostaglandins and suppress the exocrine function of the pancreas.
Blockers of histamine receptors are metabolized in the liver and excreted by the kidneys, therefore, in case of diseases of these organs, the dose should be reduced,
It should be noted that drugs in this group have a number of side effects, which are observed in 3-5% of cases. These include: dizziness, skin rash, nausea, thrombocytopenia, hemolytic anemia, hepatitis, transient impotence, genicomastia, pancreatitis. It should be remembered that all representatives of histamine receptor blockers have a withdrawal syndrome, and therefore, with the gradual withdrawal of drugs, sometimes they resort to prescribing small doses of b-blockers.
The most widely used drugs in our country are the drugs cimetidine, ranitidine (ranisan) and famotidine.
Cimetidine is one of the first drugs of this mechanism of action. During an exacerbation, he is prescribed 200 mg 3 times a day immediately after meals and 400 mg at night. There is also such a scheme of 400 mg after breakfast and before bedtime or 800 mg at night. As anti-relapse treatment, 400 mg is prescribed at night for a long time for several months or years.
Ranitidine is a more modern drug that surpasses cimetidine in its antisecretory effect. It has a higher pharmacotherapeutic activity, which allows the use of smaller single doses and in most cases avoids side effects. The scheme of administration is as follows: 150 mg after breakfast and before bedtime or 300 mg once, at night.
Famotidine is the latest generation of inhibitors of H2-histamine receptors, it surpasses the effect of cimetidine by 32 times and ranitidine by 9 times - 40 mg is prescribed once a day at night.
Now abroad there are new drugs that are superior to those listed above in their ability to inhibit the secretion of HCL - these are nizatidine and roxatidine. 2.3. Recently, a group of drugs has appeared that have carried out a "revolutionary revolution" in approaches to the treatment of peptic ulcer disease; The products of hydrochloric acid are produced. In their action, these drugs are in many ways superior to blockers of H2-histamine receptors and are practically devoid of side effects... Omeprazole is used at a dose of 30 mg once a day, after 7 days of monotherapy, acidity in the stomach disappears completely.
DRUGS STIMULATING REGENERATIVE AND TROPHIC PRO-CESSES, PROTECTING THE MUCOSA OF THE GASTRODUODENAL ZONE
1. Stimulants of mucus formation The most active drugs in this group are prostaglandins, they increase the production of bicarbonates, increase the amount of mucus. Carbenoxolone sodium (biogastron, duodenogastron), like prostaglandins, increases mucus production and changes its qualitative composition by accelerating the synthesis of glycoproteins that determine the viscosity and gelatinousness of mucus. It is prescribed in a dose of 50-100 mg 3 times a day after meals. Of the side effects, I would like to note: hypertension, fluid retention, muscle weakness, increased transaminases. 2. Drugs that promote education protective film on the ulcer surface De-nol - a preparation of colloidal bismuth is one of the most advanced drugs used for monotherapy of peptic ulcer disease. It forms a protective protein-bismuth complex with necrotic masses in the ulcer area and reduces the reverse diffusion of hydrogen ions. The effectiveness of de-nol decreases with increasing pH; therefore, the drug should not be used with medicines that reduce the activity of gastric juice. It is used 1 tablet 4 times a day 30 minutes before meals or 2 tablets in the morning and evening. It should be emphasized that de-nol is the best remedy fight against Helicobacter pilori, which is currently the primary therapeutic goal in the treatment of peptic ulcer disease. With a successful outcome of the destruction of the microorganism, all modulating factors (smoking, stress, hard physical labor, etc.) lose their significance. Venter - like de-nol, creates a film on the surface of the ulcer. It is prescribed 1 mg before meals 3 times a day and at night. 3. Drugs that improve trophism and regeneration of the mucous membrane Solcoseryl (drug from the blood of calves) - in / m 2 ml 2 times a day (2 weeks), then 100 mg 3 times a day. Methyluracil - 0.5-1.0 g 3 times a day after meals for 3-4 weeks. Gastrofarm (dried bacterial bodies of the Bulgarian lactic acid bacillus) 2 tablets crush, dissolve in a glass of water and take one hour before meals. Nerobol 1.0 IM once a week. A less pronounced trophic effect is exerted by potassium orotate, vitamins of groups A, B, C, U. In order to activate reparative processes, aloe, protein hydrolysates, FIBs, vitreous are used. Various oils (rosehip, sea buckthorn) are successfully used. It should be noted that the drugs of this group are not used as monotherapy for peptic ulcer disease and can be used as adjuvants.
MYOTROPIC SPASMOLITICS - are prescribed for severe pain syndrome in combination with M-cholinolytics, they reduce the tone of the pylorus and reduce the contractile activity of the smooth muscles of the stomach and duodenum. The most commonly used drugs are: papaverine hydrochloride, no-spa, halidor in usual therapeutic dosages. I would especially like to note raglan or cerucal - a drug that has a normalizing effect in any violation of the motor activity of the gastrointestinal tract, is prescribed for severe dyspepsia - vomiting, hiccups, nausea, belching 2 ml / m 2 times a day or 1 tablet (10 mg) 3-4 times a day.
DRUGS ACTING ON THE CENTRAL NERVOUS SYSTEM have not lost their relevance, given the cortico-visceral theory. Eglonil - refers to central anticholinergics and neuroleptics, has an antiemetic, anti-nausea effect and is a mild depressant. It reduces the motor activity of the stomach, relieves the pylorus spasm, improves the evacuation function of the stomach and duodenum, and increases the blood supply to this zone. Under the influence of the drug, the feeling of anxiety goes away, sleep improves, appetite is normalized, pain syndrome is stopped. In the exacerbation phase, 2.0 (100 mg) intramuscularly is prescribed, 2 times a day for 2 weeks, then they switch to oral administration - 1 capsule (50 mg) 3 times a day. Gastrobomat - has a similar effect, with a slightly more pronounced hypnotic effect, 2-4 tablets are prescribed 3 times a day, before meals, for 3-4 weeks. The appointment of sedatives (diazepam), tranquilizers (seduxen, elenium, tazepam), and sometimes antidepressants is shown. All of these drugs reduce the basal secretion of hydrochloric acid and have an antispasmodic effect, but their purpose is to improve the functional state of the nervous system. Drugs acting on the central nervous system do not have an independent significance in the treatment of peptic ulcer disease and are prescribed only in combination with antacids.
PHYSIOTHERAPY should be prescribed depending on the phase of the disease and the severity of the inflammatory process. So, in the exacerbation phase, it is shown: sinusoidal modulated currents or DDT (10-12 procedures) then switch to ultrasound or microwave therapy. A good effect is obtained from electrosleep. Phase of fading exacerbation - mud, peat, ozokerite-paraffin applications on the epigastric region, UHF, electrophoresis with novocaine, papaverine. As sedatives, they resort to the appointment of hydrotherapy: coniferous, pearl, oxygen and radon baths. In sanatorium-resort conditions, mud therapy is successfully applied, applications from silt mud or peat are prescribed low temperatures(38? C). These procedures reduce hypersecretion, normalize motor function, and improve blood circulation in the mucous membrane of the gastroduodenal zone.
TACTICS OF APPLICATION OF PHARMACOLOGICAL DRUGS The choice of drugs depending on the form of the disease is made taking into account the prevalence of hydrochloric acid hypersecretion and hypermotility of the gastrointestinal tract in duodenal ulcer disease, and in case of gastric ulcer - violations of the protective barrier of the mucous membrane and reinfusion of hydrogen ions. Therefore, with duodenal ulcer localization, preference should be given to powerful antisecretory agents antacids, M-anticholinergics and H2-histamine receptor blockers. With the localization of an ulcer in the stomach, adsorbents, gastrocepin are more often prescribed, from means that regulate motility, eglonil and cerucal are shown, if necessary, resort to the use of metacin and peritol.
Carbenoxolone sodium, de-nol and gastrocepin are equally effective in any localization of the process. For any form of peptic ulcer, the use of sedatives and drugs that improve trophism is indicated. When Helicobacter pilori is detected, the classic "triple therapy" is used, consisting of a combination of bismuth subcitrate or subsalicylate, metranidazole and tetracyclines, or a combination of omeprazole with amoxicillin. The most effective is the "Italian" weekly regimen, consisting of 20 mg of omeprazole, 2 times a day, 400 mg of metranidazole and 2 times a day, 250 mg of clarithromycin. Treatment of exacerbations of peptic ulcer disease lasts on average 2-3 months, with the onset of remission, preventive treatment is carried out, which is carried out 2 times a year for 1.5-2 months. With a frequently recurrent course, year-round treatment is carried out for 1-2 years. As a rule, this is monotherapy with one of the following drugs: omeprazole (20 mg at night), gastrocepin 50 mg (2 tablets at bedtime), De-nol (1 tablet before breakfast and 1 after dinner), sucralfate (1 tablet before breakfast and 1 after dinner), ranitidine (150 mg at bedtime), cimetidine (200-400 mg at bedtime). As already mentioned, in order to enhance the therapeutic effect, the combined use of antiulcer drugs is often used. It was said about rational combinations earlier, in conclusion it is necessary to dwell on undesirable schemes.
1. It is irrational to combine M-anticholinergics with cerucal and eglonil.
2. In case of gastric ulcer the activity of de-nol decreases when combined with antisecretory drugs.
3. The bioavailability of cimetidine decreases when combined with antacids. Absolute indications for surgical treatment are long-term non-scarring callous ulcers, ulcer repetition and repeated bleeding. As for the relative indications, this issue requires further joint study, but for now surgeons operate on patients who could still be treated conservatively, and therapists prescribe drug treatment to those patients who should already be operated on.