Oral diseases can cause various reasons. These include dental problems and diseases. internal organs, and damage (for example, hot or spicy food), and general dehydration, vitamin deficiency, as well as many other factors. All diseases that can occur in the human mouth can be divided into viral, infectious-inflammatory and fungal diseases. In addition, there are several unpleasant ailments that cannot be classified into any of these groups. In order to choose the right specialist to whom you need to contact with a particular problem, as well as in order to know which disease you can treat yourself and how, and which you cannot, you need to know each of the oral diseases “in person”.
Viral diseases
Viral diseases in oral cavity Humans can be caused by the herpes virus and the human papilloma virus.
Herpes is one of the most common diseases. It is believed that ninety percent of people are infected with this virus.
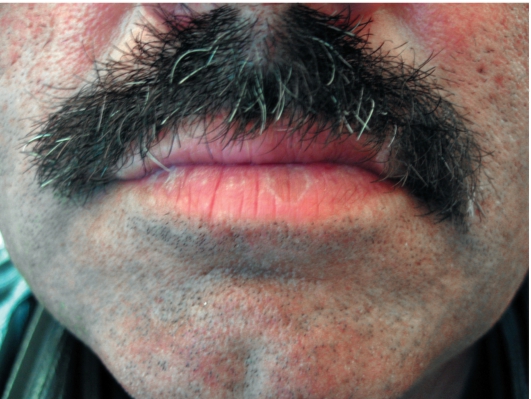
An example of herpes on the lips.
Often this virus is located in the body in a latent form. In a strong person, it can manifest itself only as a small pimple on the lip, which dies off without outside help within one to two weeks, but in a weakened person, herpes manifests itself much more significantly.
Calm herpes can be triggered into action by factors such as stress, surgery, colds, fever, lack of sleep, wind, cold, menstruation, and immunosuppression.
Herpes usually develops in stages, going through six stages. It all starts with itching and tingling on the lips and adjacent tissues, after which the lips swell, turn red, pain appears, making it difficult to eat and speak, followed by the appearance of single blisters or entire groups of blisters. After some time, the blisters burst and turn into small ulcers. The ulcers become covered with a hard crust that may crack. In the final stage, the ulcers gradually disappear, redness and pain disappear.
At the first symptoms of herpes, you need to apply ice to your lips and moisturize them with special balms. The bubbles that appear are lubricated with a special ointment that can be bought at a pharmacy without a prescription (for example, Penciclovir or Abreva). If a person is prone to too frequent exacerbations of herpes, the doctor may prescribe antiviral drugs.
Papilloma
Human papilloma can occur in various parts of the body, but one type of human papillomavirus can cause papillomas to appear in the oral cavity. In the mouth, these sores look like cauliflower, that is, plaques appear white.
The most unpleasant consequences of this disease occur when it reaches the throat, because it can cause not only hoarseness, but also difficulty breathing.
Unfortunately, it is impossible to completely cure the human papillomavirus, so treatment consists of eliminating clinical manifestations. If we talk about the treatment of this virus in general outline, then it comes down to choosing one of the methods: surgical, chemical, cytostatic, immunotherapy or a combination of the above methods.
Infectious and inflammatory diseases
Infectious diseases of the oral cavity are the most common problem for which people turn to dentists, otolaryngologists or therapists. This type includes pharyngitis, gingivitis, etc.
Pharyngitis is an inflammation of the mucous membrane of the pharynx and, in particular, the throat. As a rule, it is accompanied by soreness, discomfort and severe pain throat.

Acute pharyngitis.
Pharyngitis can be caused by various factors: inhalation of cold or polluted air, tobacco smoke, various chemical pollutants. In addition, pharyngitis can also be caused by an infection (pneumococcus).
To the symptoms of pharyngitis already listed above (discomfort, sore throat and sore throat), you can also add general malaise and fever (the latter is typical only for acute pharyngitis, but not for chronic).
Diagnosed this disease general examination and throat swab. Doctors treat pharyngitis with antibiotics only in difficult cases; as a rule, all that is needed is a special diet, hot foot baths, warm compresses on the neck, warm milk with honey, inhalations and rinses.
Glossitis
Glossitis is an inflammatory process. It changes the structure as well as the color of the tongue. It is caused by oral infections. Glossitis can be provoked by a burn of the tongue, excessive love of hot drinks, trauma to the oral cavity and tongue, because all this is a kind of “pass” for infection. In addition, those who abuse alcohol, spicy foods and mouth fresheners are at risk. Of course, those who neglect oral hygiene, in particular, use other people's toothbrushes, also have an increased chance of getting glossitis.
The first symptoms of the disease are a burning sensation and discomfort; a little later, the color of the tongue becomes bright red and salivation increases. Further symptoms include dullness (or complete absence) of taste sensations. Although it has been noticed that sometimes the sensation of tastes does not disappear, but is distorted.
If there is no treatment for this infection, the swelling of the tongue reaches such proportions that it becomes very difficult for a person to speak and eat, in addition, the tongue itself becomes covered with growths.
Treatment for glossitis is prescribed by the dentist. It consists of taking medications and a special diet based on semi-liquid food.
Gingivitis is characterized by inflammation of the gum lining. This is a fairly common disease that affects teenagers and pregnant women the most.
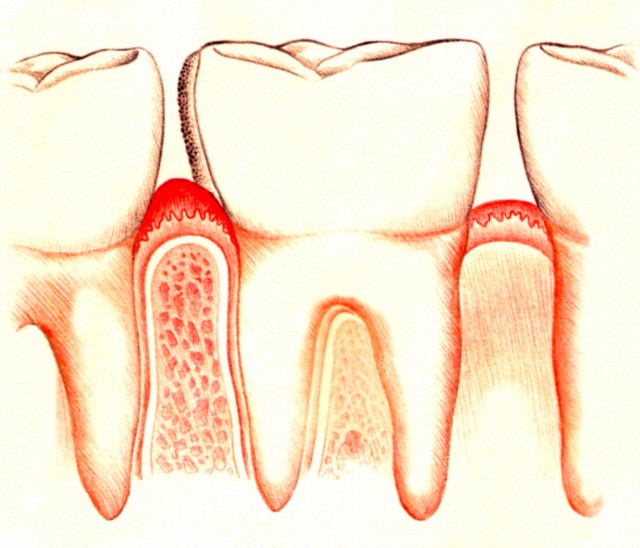
Gingivitis affects the gums.
There are four types of this disease: catarrhal gingivitis, ulcerative-necrotic, hypertrophic, atrophic.
- catarrhal gingivitis is characterized by symptoms such as redness and swelling of the gums, itching and bleeding;
- with ulcerative necrotic gingivitis, ulcers and necrotic areas appear on the gums, in addition, symptoms characteristic of this disease are: bad smell from the mouth, severe pain, general weakness, fever and enlarged lymph nodes;
- hypertrophic gingivitis enlarges the gingival papillae and covers part of the tooth with them, in addition, slight bleeding of the gums and mild pain are possible;
- with atrophic gingivitis, a person begins to react sharply to hot and cold, the level of the gums decreases, and the tooth becomes exposed.
The dentist can quickly and painlessly cure gingivitis if you contact it in the early stages, and the doctor will also give recommendations on oral hygiene to avoid this disease in the future.
Stomatitis
If we talk about infectious diseases oral cavity, the most common of them is stomatitis.
It is possible for infection to enter the body different ways, for example, due to mechanical trauma. After infection, a person develops special ulcers that are characteristic only of stomatitis. They are localized on inner surface cheeks and lips, at the root of the tongue, as well as under it. Have ulcers next view: shallow, single, round, the edges are smooth, and the center is covered with a film, as a rule, the ulcers are very painful.
When treating this disease, it is necessary to use special toothpastes and mouth rinses that do not contain sodium lauryl sulfate. To relieve the pain of ulcers, anesthetic drugs should be used. In addition, there are special drugs that help remove the harmful film from ulcers, which speeds up treatment. And, of course, you cannot do without anti-infection medications that your doctor will prescribe for you.
How to distinguish herpes from stomatitis?
Sometimes it is very easy to confuse a viral infection that is caused by an infection, because in both cases painful sores appear in a person’s mouth. There are three characteristic differences between these diseases:
- herpes always appears in the same place, while stomatitis always chooses new affected areas;
- herpes always affects those areas of tissue that are adjacent to the bones; stomatitis “likes” soft tissue more;
- During herpes, ulcers appear due to the bursting of small blisters, and stomatitis initially begins with ulcers.
Fungal diseases
Half the population globe are inactive carriers of Candida fungus. It can be activated if the body's immune defense is weakened. Candidiasis (a disease caused by Candida) comes in several types.
The most common is thrush. Its symptoms are dryness and white coating inside the cheeks and lips, on the palate and back of the tongue. All this is accompanied by a burning sensation and severe discomfort, and children tolerate thrush much easier than adults.
Most sickly look candidiasis – atrophic. The mucous membrane of the oral cavity acquires a bright red color and becomes dry. With hyperplastic candidiasis, a thick layer of plaque appears, and when you try to remove it, the surface begins to bleed.
This kind fungal disease, as atrophic candidiasis usually provokes long-term wearing of lamellar dentures. The mucous membrane of the tongue, palate and corners of the mouth dries out and becomes inflamed.
Treatment for the disease “candidiasis” can only be prescribed by a doctor, because it is extremely important to correctly determine its type, and for this you need to conduct a whole series of tests.
Lichen planus is another type of fungal disease. It causes plaques, blisters, ulcers and redness in a person's mouth. As a rule, lichen is combined with diseases such as diabetes, stomach and liver diseases.
Other diseases
In addition to the above diseases, there are several that are difficult to classify into one group or another. For example, geographic language, a completely safe disease (although it is difficult to call it a disease, rather a change) of the language. In this case, the tongue is covered with a kind of grooves, reminiscent of a geographical map.
But among the unclassified diseases, there is one that is still worth paying attention to - oral dysbacteriosis. The cause of this disease is the use of various antibiotics and antiseptics during the treatment of other problems.
Symptoms of dysbiosis begin with minor ones - cracks in the corners of the lips, unpleasant odor from the mouth and lead to loosening of teeth and damage to their enamel. To overcome dysbiosis, it is necessary to restore the healthy microflora of the oral mucosa.
© phanuwatnandee / Fotolia
The inflammatory process that occurs on the mucous membranes of the oral cavity, manifested in the formation of ulcers, blisters, or even just a whitish coating, is most often diagnosed as stomatitis.
Until recently, the disease predominantly affected children’s bodies, but there was a widespread decrease in the population’s immunity, deterioration environmental situation and many other associated factors contributed to the widespread spread of the disease among adults. Therefore, it is so important to know and take timely measures to treat stomatitis and prevent it.
Root causes
More often the development of stomatitis in adults occurs due to the active action of bacteria, viruses or infections. Such a turn of events is possible only with reduced immunity due to the occurrence of diseases of other organs and systems of the body (diseases of the oral cavity, chronic diseases of the gastrointestinal tract, upper respiratory tract, HIV, oncology, etc.).
In addition, the active proliferation of pathogenic microorganisms on the oral mucosa can be provoked insufficient attention to personal oral hygiene(using someone else’s toothbrush, drinking drinks from the same bottle, ignoring them, etc.).
The lack of certain microelements in the body due to poor-quality or unbalanced nutrition (B vitamins, zinc, iron, folic acid) can also lead to the appearance of characteristic ulcers on the oral mucosa.
Another common factor that provokes the occurrence of stomatitis is trauma to the tissues of the oral surface. Patients often themselves note that plaque and ulcers in the mouth occur at the site of accidental damage to the mucous membrane (scratches on a tooth fragment, crown or denture, cheek bite, damage from solid food, burns, exposure to chemicals).
Of course, trauma to the oral cavity does not always lead to the appearance of stomatitis, but in combination with other factors, such an outcome is quite possible.
Symptoms of the disease

© charnsitr / Fotolia
Stomatitis manifests itself by the occurrence swelling and painful inflammation, accompanied by a burning sensation. Soon, a single oval or round ulcer with a red halo around it will form in this place.
The patient is bothered by painful sensations, increased salivation and bad breath. There are certain difficulties with chewing food and speaking. Acute forms of the disease can occur with an increase in body temperature to 39 0.
What can you do at home?
Treatment of stomatitis at home can give positive dynamics if you approach the process with full responsibility and regularly treat all ulcers and blisters:
- Will provide all possible assistance in the treatment of stomatitis in adults hydrogen peroxide. You need to dilute one teaspoon of peroxide in 1/2 cup boiled water, and rinse your mouth three times a day. This procedure will help get rid of pain.
- Garlic-sour cream mixture among the means to combat stomatitis at home, I received very good feedback. The garlic must be finely grated and mixed with a small amount of sour cream. This composition is kept in the mouth for half an hour 2-3 times a day.
- Stomatitis safely “loses its ground” even with regular rinsing the mouth with vegetable juices (cabbage or carrots). Freshly squeezed juice is mixed with water in a ratio of 1/1 and rinsing procedures are carried out three times a day.
- Relieves inflammation well even in advanced cases onion peel decoction. To prepare it, use onion peel (5 tablespoons) and 500 ml. water. The husks must be boiled for 15 minutes, then cooled and left to steep overnight.
The finished broth is filtered, boiled water is added, bringing the total volume to the original 500 ml, and used for its intended purpose: rinse the mouth with it three times a day.
Any of the listed activities must be accompanied by the consumption of fruits and vegetables to provide the body with vitamins and beneficial microelements that stimulate the immune system.
These methods will certainly help in isolated cases, however, if the appearance of stomatitis recurs periodically, complex treatment and consultation with a specialist will most likely be required.
Use of folk remedies

© samiramay / Fotolia
Stomatitis is a disease that has quite a ancient history, therefore it is not surprising that traditional medicine knows a lot effective ways fight against this disease.
Decoctions of medicinal plants can significantly alleviate the situation until complete recovery.
- Oak bark has anti-inflammatory properties. To obtain a healing potion, you need to cook 1 tbsp over low heat for 10 minutes after boiling. spoon of bark in a glass of water.
Rinse with strained and cooled broth up to five times a day. The indicated rate is for one rinse only. For convenience, you can prepare the decoction for the whole day at once.
- Aloe– excellent folk remedy, which also helps with stomatitis. To obtain a therapeutic effect, it is necessary to squeeze a small amount of juice from the leaves of the plant and treat the damaged area of the mucous membrane with it (using a regular pipette). This procedure must be repeated up to 3 times a day.
- IN summer period can be used to treat stomatitis plantain juice. To do this, you need to collect fresh leaves, wash them well, grind them in a meat grinder and squeeze them through cheesecloth. The resulting liquid is used to treat ulcers and blisters.
And one more folk recipe to combat stomatitis - a decoction of burdock. How and in what proportions to prepare it - see the following video:
What medications can be used
In medicine, it is customary to distinguish several types of stomatitis. Depending on the type of disease, certain drugs are prescribed to combat it:
Antiseptic
Ambazon (pharyngosept). A drug that has a bacteriostatic effect. Prescribed for treatment and preventive measures to combat inflammatory formations in the oral cavity.
Hexasprey. Biclotymol – main active substance this drug. Has an antiseptic effect. Excellent for disinfecting the entire oral cavity.
What should you do if? We have the answer to this question!
In this article you will find out whether it is true or not that the reason for grinding your teeth in your sleep is worms.
Antifungal
Weakened the immune system unable to resist the development of candidiasis. This usually occurs against the background of serious diseases of systems and internal organs, accompanied by the use of large quantity antibiotics. In this case, the following will help to cope with stomatitis:
Diflucan (fluconazole). Available in capsule form, it is prescribed for any form of candidiasis.
Levorin. In fact, this drug is also an antibiotic with an antifungal effect. You can purchase it in the form of an ointment or a special lyophilisate for preparing a rinse solution.
Candide. A drug wide range actions.
Antiviral

© Max Tactic / Fotolia
Oxolinic ointment. Antiviral drug. Actively resists herpes viruses, influenza, adenovirus. Available in the form of an ointment that must be applied to the affected areas.
Viru-merz. Created to combat the herpes virus. Reduces the duration of treatment several times.
Acyclovir. A widely known antiviral drug used to combat herpes stomatitis. Zovirax, acigerpin, gervirax, and vivorax are offered as analogues.
Antihistamines
Allergic stomatitis is another manifestation of a disease of the oral mucosa associated with a certain reaction of the body to certain allergens. The following drugs are prescribed as treatment: tavegil or its analogues, fenkarol.
Antibiotics
IN in rare cases acute forms Antibacterial drugs are prescribed for stomatitis: chlorhexidine bigluconate, sumamed, amoxiclav, augmentin.
In addition, along with substances that act directly on the source of the disease, drugs are used that promote the healing of damaged tissues: Solcoseryl, Karotolin, Propolis spray.
Stomatitis on the tongue
Depending on the nature of the occurrence of stomatitis in the tongue, it can be treated independently with home remedies or recipes traditional medicine, or with the help of medications prescribed by a specialist after a thorough examination.
Rinsing with decoctions of chamomile, calendula, and linden flowers will help disinfect and speed up wound healing. Raw potato juice.
To avoid acute painful sensations, it is necessary to follow a certain diet - avoid spicy, sour, use of various spices, and, if possible, salt and sugar. Fresh food should be taken only in a mushy state at room temperature.
Prevention

© Voyagerix/Fotolia
The most important rule for preventing stomatitis is maintaining oral hygiene. Using a toothbrush and toothpaste twice a day is mandatory.
To help these hygiene products add dental floss and rinsing with antibacterial solutions. Of course, you should not ignore visits to the dentist and sanitize your oral cavity in a timely manner.
A healthy and balanced diet is the basis for a strong immune system, so it is important to watch what and when you eat. If there is a lack of vitamins, it is recommended to take a course of vitamin-containing medications several times a year..
And the main thing, of course, is not to start the disease. And even if you find signs of stomatitis, you must immediately apply comprehensive measures to eliminate the disease, including rinsing with healing decoctions, using antiviral and antibacterial drugs, and measures to strengthen the immune system.
Good health to you!
If you find an error, please highlight a piece of text and click Ctrl+Enter.
Chapter 11. DISEASES OF THE ORAL MUCOSA. CHEILITIS
Chapter 11. DISEASES OF THE ORAL MUCOSA. CHEILITIS
Cheilites (cheilitis)- a group of benign inflammatory diseases of the lips.
Conventionally, cheilitis can be divided into 2 groups: primary cheilitis, which occurs as an independent disease, and symptomatic cheilitis, which are signs of other diseases.
11.1. PRIMARY CHEILITIS
Contact cheilitis
Distinguish simple contact cheilitis And allergic contact cheilitis. The etiology and pathogenesis of these forms are different. There are obligate and facultative causal factors.
Obligate factors cause cheilitis in any person; optional- only in persons who are hypersensitive to a specific allergen.
Simple contact cheilitis
Simple contact cheilitis is a lesion of the lips that occurs after contact of the mucous membrane of the lips with an obligate irritating factor (physical, chemical, biological nature). This lip lesion develops in all people, and the degree of damage to the mucous membrane directly depends on the strength of the irritating agent.
Obligate factors: chemical irritants (acids, alkalis, detergents, solvents, soaps, etc.); mechanical stimuli (pressure, friction); tall and low temperatures; UV and ionizing radiation; biological irritants (plants - spurge, buttercup, etc.; caterpillars, some insects), saliva (with prolonged exposure to the skin).
Depending on the strength and frequency of exposure to the irritating factor, as well as its nature, the effect on the skin may be different.
When exposed to a weak irritating factor (water, saliva, soap in combination with unfavorable weather conditions), the skin epidermal barrier is destroyed and subacute or chronic inflammatory reactions are formed, caused by the penetration of antigens into the mucous membrane of the lips.
Most often occurs simple cheilitis, which develops as a result of constant licking and biting of lips (sometimes of an obsessive nature), often in winter time of the year. Common in children younger age and in teenagers. Clinically, cheilitis is characterized by dry, cracked lips covered with small scales, accompanied by severe itching.
Frequent manifestation of contact cheilitis - meteorological cheilitis, the causes of which may be high or low humidity, wind, cold, dusty air, solar radiation. This type of cheilitis is typical for people with fair and delicate skin, as well as for patients who have increased dry skin (ichthyosis, atopic dermatitis, etc.)
In case of exposure of the mucous membrane to strong aggressive external factors destruction of cells of the epidermis, dermis, as well as deeper tissues occurs, the formation of necrosis. The course of the disease is acute.
Depending on the concentration and duration of exposure to the irritating factor, either erythema, a bubble, or a scab may form on the mucous membrane. Characterized by a clear boundary of the lesions. When the influence of the irritating factor on the mucous membrane ceases, the inflammatory reaction gradually resolves independently.
Contact allergic and eczematous cheilitis
The development of allergic contact and eczematous cheilitis is based on an inflammatory immune reaction that develops on the mucous membrane of the lips after contact with an allergen. Rarely occurs in children under one year of age.
Allergens can be a wide variety of chemical substances that are found in everyday life, production, and nature. The most common causes of contact-allergic cheilitis are lipsticks, cosmetic creams, pastes, chewing gums, fruits (citrus fruits, pineapples, etc.), writing instruments, etc.
(Figure 11-1).
Rice. 11-1. Allergic cheilitis
The pathogenesis of cheilitis includes the phase of primary contact with the allergen (sensitization) and the phase of repeated exposure of the allergen to the skin with the development of clinical manifestations (dermatitis) in all areas of the mucous membrane of the lips and skin who have ever been sensitized to this allergen. The disease is the result of a cell-mediated delayed-type allergy (type 4 reaction) with the characteristic participation of the epidermis - the formation allergic reaction eczematous type. The time of sensitization ranges from several days to several months and years.
Clinical picture
The clinical picture is characterized by the appearance of erythema with fuzzy edges, vesicles, serous crusts, and scales. Over a long period of time, the red border of the lips becomes dry and multiple cracks appear on it (Fig. 11-2). Patients are bothered by severe itching.
A type of eczematous cheilitis - microbial eczema of the lips, which develops during a long course of the infectious process on the lips or on the facial skin of the perioral area (microbial seizure, chronic fissure of the lips, facial pyoderma, chronic rhinitis, etc.). The eczematous reaction is most pronounced near the microbial focus (Fig. 11-3).

Rice. 11-2. Eczematous cheilitis

Rice. 11-3. Microbial cheilitis
Treatment
The basis of treatment is the elimination and cessation of the action of the provoking factor. Topical glucocorticoids (hydrocortisone ointment, alklometasone, methylprednisolone aceponate, hydrocortisone, etc.) are prescribed externally 1-3 times a day for 2-5 days.
For meteorological cheilitis, it is recommended to regularly use emollient nourishing creams and balms that reduce dry lips and have a protective effect (hygienic lipsticks, cold lip creams, ceralip lipsticks, atoderm, etc.).
For microbial eczema of the lips, combined glucocorticoid agents are externally indicated (hydrocortisone ointment + oxytetracycline, hydrocortisone cream + natamycin + neomycin, hydrocortisone aerosol + oxytetracycline, etc.)
Exfoliative cheilitis
Exfoliative cheilitis is an inflammatory disease of the red border of the lips with a genetic predisposition, belonging to the group of psychosomatic diseases. This cheilitis is more common in children and young. Clinically, two forms of the disease are distinguished: exudative and dry. Mark the transition from one form to another.
Neurogenic mechanisms play an important role in the pathogenesis of this cheilitis. It is believed that with the exudative form of the disease in patients, anxiety states, and when dry - depressive.
Clinical picture
At exudative form Due to the increased permeability of capillaries, large scaly crusts appear on the red border of the lips, the place of attachment of which is the line where the lips close (Klein line), covering only half of the lip. The process never transfers to the skin. After removing the crusts, the bright red, smooth (not eroded) surface of the red border of the lips is exposed (Fig. 11-4).
At dry form on the red border of the lips along the Klein line, multiple white-gray scales appear, tightly attached in the central part and resembling resin.
Treatment

Rice. 11-4. Exfoliative cheilitis in a patient with Down syndrome
corticoid ointments and creams. In the dry form, the use of nourishing balms, hygienic lipsticks, and indifferent ointments is indicated.
Actinic cheilitis
Actinic cheilitis is a chronic disease that is caused by increased sensitivity of the red border of the lips to sunlight.
The main reason for the occurrence of this cheilitis is the development of a delayed-type allergic reaction to UV rays. The disease is characterized by seasonality: spring-summer.
Clinical picture
The lesion is more pronounced on the lower lip. Clinically, the disease occurs in two forms: dry And exudative. In the dry form, the red border of the lips becomes bright red, covered with many small scales. In the exudative form, the lesions on the lips resemble manifestations of allergic contact dermatitis (hyperemia, vesicles, crusts). With a long course of the disease, whitish papules (leukoplakia) and erosion appear on the lips.
A special form of chronic actinic cheilitis - abrasive precancrosis cheilitis Manganotti, which occurs most often in

Rice. 11-5. Heilith Manganotti
older men. The disease is considered an obligate precancer. Clinically characterized by the appearance on the red border lower lip erosive areas with a smooth shiny surface (“polished with abrasive”), without crust (Fig. 11-5). The course is long and persistent. The prognosis in some cases is unfavorable.
Treatment
Sun exposure should be avoided (in spring-summer time mandatory use of creams and balms with high degree photoprotection). In case of severe damage to the lips, courses of vitamin therapy (vitamins B2, B6, B12), antimalarial drugs, and low doses of glucocorticoids are prescribed. Glucocorticoid creams and ointments are indicated externally.
Glandular cheilitis
Glandular cheilitis is a chronic disease of the red border of the lips, resulting from heterotopia (atypical arrangement of glands on the red border of the lips), hyperplasia (increase in size) and hy-
perfunction (increased secretion) of small salivary glands. This disease appears after puberty.
Clinical picture
The disease is characterized by the appearance of red dots (the mouths of the salivary glands) on the red border of the lips, from which droplets of saliva are released. Frequent wetting of the red border of the lips with saliva leads to dryness and the formation of chronic cracks. The addition of a secondary infection entails the development of a purulent form of glandular cheilitis. With a long course of this cheilitis, the development of leukoplakia around the heterotropic salivary glands is also possible.
Treatment
Heterotopic salivary glands are removed using electrocoagulation or laser destruction.
Chronic recurrent lip cracksChronic median fissure of the lip
A chronic fissure of the lip is a long-term, vertically located defect of the lower lip that occurs against the background of decreased tissue elasticity.
For the development of chronic lip fissures great importance has its individual structure (deep fold in the center of the lip), less often - a chronic injury. Loss of elasticity also develops when exposed to various meteorological factors, against the background of chronic skin diseases accompanied by xerosis. In children, a chronic cracked lip often occurs when they have the habit of breathing through the mouth due to difficulty passing air through the upper Airways(deviated nasal septum, adenoids).
Clinical picture
The clinical picture is typical and most often represents a single crack on the lower lip in its middle part (less often on the side) (Fig. 11-6). The depth of the crack can vary (from superficial to deep), but it never extends to the skin around the lip. At night, a shallow crack may begin to epithelialize, but in the morning, when you move your lip, it opens again and can bleed.

Rice. 11-6. Chronic fissure of the lower lip Treatment
If possible, determine and eliminate the cause of the disease (restoration of lip architecture, elimination of mouth breathing, etc.). External treatment begins with the prescription of weak glucocorticoid agents in combination with antibacterial drugs (hydrocortisone ointment + oxytetracycline, hydrocortisone + oxytetracycline, hydrocortisone cream + natamycin + neomycin, etc.), as well as regenerating agents (methyluracil* ointment, Actovegin*, solcoseryl* and etc.). If there is no healing, helium-neon laser therapy or surgical excision of the crack within healthy tissue is recommended.
Seizures (angular cheilitis)
The most common causes of jamming: chronic allergic diseases of the lips, leading to a decrease in the elasticity of tissues (eczematous cheilitis, atopic cheilitis, etc.), infections (streptoderma, candidiasis, PG, etc.), excessive salivation, impaired oral architecture (malocclusion, poor prosthetics, etc.).

Rice. 11-7. Seizures
Clinical picture
The clinical picture is manifested by erosions and linear cracks in the corners of the mouth (Fig. 11-7).
Treatment
In most cases, external use of combined glucocorticoid drugs (hydrocortisone + oxytetracycline ointments, fusidic acid + hydrocortisone, hydrocortisone + oxytetracycline, hydrocortisone + natamycin + neomycin, etc.) has a good therapeutic effect.
11.2. SYMPTOMATIC CHEILITIS
Atopic cheilitis
Atopic cheilitis is the most common type of lip lesions in children and adolescents. Atopic cheilitis is one of the symptoms of atopic dermatitis, and during remission it may be its only manifestation.
Clinical picture
Atopic dermatitis affects the red border of the lips, especially the corners of the mouth, and the surrounding skin. The red border of the lips is infiltrated, peels off in small scales, its entire surface is cut by thin radial grooves (Fig. 11-8). Patients are bothered by severe itching. Even after the inflammatory phenomena have subsided, tissue infiltration and radial folds (“fan”, “accordion”) remain for a long time in the corners of the mouth.
Treatment
In the acute stage, glucocorticoids (hydrocortisone, alklometasone, hydrocortisone + oxytetracycline, etc.) are used externally for a short course. In the subacute and chronic stages, softening nourishing creams-balms are prescribed that reduce dry lips (hygienic lipsticks, cold lip creams, Ceralip lipsticks, Atoderm, etc.).

Rice. 11-8. Atopic dermatitis
Rice. 11-9. Lichen planus
Lip damage due to lichen planus
Damage to the lips with lichen planus is common and manifests itself as small papules of a whitish-pearly color on the mucous membrane, which, merging, form bizarre patterns (“fern leaf”, “mesh”) (Fig. 11-9).
Damage to the lips due to pemphigus
Damage to the lips in pemphigus is one of the main clinical signs of this disease. It is characterized by the appearance of blisters in the oral cavity and on the red border of the lips, which quickly open and leave behind long-term non-healing erosions.
With lupus erythematosus, spots appear on the lips, covered with silvery, tightly fitting scales, erosion, and later cicatricial atrophy develops. Observe the transition of the lesion from the red border of the lips to the skin around the lips (Fig. 11-10).

Rice. 11-10.Lip damage due to lupus erythematosus
Lip damage due to specific diseases
Damage to the lips can be observed in patients with syphilis (chancroid, macular or papular syphilis); tuberculosis (primary tuberculous ulcer, tuberculous lupus, miliary ulcerative tuberculosis), chancriform pyoderma, scleroderma, ichthyosis and other dermatoses.
Drug-induced cheilitis
Drug-induced cheilitis is a lesion of the lips that develops while taking medications.
Clinical picture
Most often, cheilitis is observed with toxicoderma. This lesion is especially characteristic of exudative erythema multiforme, Stevens-Johnson syndrome and Lyell's syndrome, in which erosions appear on the lips, covered with black and red hemorrhagic crusts. In acute urticaria and angioedema, the appearance of urticarial elements and an increase in the size of the lips are noted. Medi-
Kamentous cheilitis can also develop after direct contact of a medicinal substance with the red border of the lips (potions, syrups, inhalants, vasoconstrictor drops, etc.) and is clinically characterized by the appearance of contact cheilitis.
Treatment
Treatment is aimed at the underlying disease. External therapy - as in persons with atopic dermatitis.
Chronic recurrent aphthous stomatitis
Recurrent aphthous stomatitis is a chronic inflammatory disease characterized by the appearance of painful ulcers on the oral mucosa and occurring with periodic remissions and exacerbations. Often occurs in children after 3 years of age.
Etiology and pathogenesis
Among the predisposing factors highest value have a hereditary predisposition, food allergies, trauma, stress, functional disorders of the gastrointestinal tract (biliary dyskinesia, constipation, diarrhea). Recurrent aphthous stomatitis can also be a manifestation of some systemic diseases (Crohn's disease, Behçet's disease, ulcerative colitis, etc.).
In the pathogenesis, the main role is assigned to immunological disorders (especially cell-mediated immunity).
Clinical picture
The disease often begins with a prodromal period, which is characterized by the appearance of unpleasant sensations in the oral cavity, erythema, at the site of which a defect (aphtha) is formed.
Aphtha is a superficial painful ulceration of the oral mucosa with a diameter of 3-5 mm, round or oval, covered with fibrinous plaque and surrounded by a hyperemic edematous rim (Fig. 11-11). Patients often develop multiple aphthous rashes, in which articulation and eating are difficult due to severe pain. The favorite localization of aphthae in children is the anterior part of the oral cavity, the mucous membrane of the lips, the transitional fold of the upper and lower lips, and the lateral surfaces of the tongue. The healing period for aphthae is 7-10 days without scarring.

Rice. 11-11. Aphtha
Depending on the severity, there are 3 forms of chronic recurrent aphthous stomatitis.
The mild form is single aphthae, low-painful, recurrent once every few years.
Moderate form - relapses 1-3 times a year.
Severe form - relapses occur more than 4 times a year, sometimes monthly or continuously.
Features of the course of aphthous stomatitis in children
In newborns, there may be signs in the oral cavity Bednar's aphthae:“sucking ulcers” are trophic ulcers of traumatic origin, localized only at the border of the soft and hard palate, formed due to difficulty sucking.
If you cough frequently with your tongue hanging out (for example, with whooping cough), ulcers may form on the frenulum or the lower surface of the tongue - aftas Fede-Rici.
Differential diagnosis
Differential diagnosis is carried out with herpetic stomatitis, traumatic ulcers, viral pemphigus of the oral cavity and extremities, secondary syphilis, erythema multiforme, and pemphigus.
Treatment
Before starting therapy, it is necessary to examine the patient and exclude systemic diseases in which aphthae may be one of the clinical symptoms.
Consultation with a gastroenterologist and scatological examination are necessary. If necessary, regulate intestinal activity and eliminate constipation.
Objectives of local treatment
Reducing pain: applications of local anesthetics (2% solution of lidocaine, benzocaine, etc.).
Reducing the healing time of aphthae. Applications with proteolytic enzymes, a concentrated solution, have a cleansing effect table salt, sugar syrup, honey. Anti-inflammatory drugs are prescribed - hexetidine solutions, choline salicylate gel + cetalkonium chloride, metronidazole jelly + chlorhexidine, local use of glucocorticoid drugs on an adhesive basis. Products with regenerating properties are also prescribed: solcoseryl * dental adhesive paste, oil solution of 10% retinol, sea buckthorn oil, vinylin, etc.
Consulting
The patient needs to be explained possible reasons lesions of the mucous membranes of the oral cavity and lips, the role of internal pathology and underlying dermatosis.
Dermatovenerology: a textbook for higher education students educational institutions/ V. V. Chebotarev, O. B. Tamrazova, N. V. Chebotareva, A. V. Odinets. -2013. - 584 p. : ill.
Oral diseases are very common. Suffice it to say that they occur in almost all adults and 70 percent of children. Most are characterized by pathological processes of an inflammatory nature.
The oral mucosa is reliable protection body and has a close connection with a number of internal organs and systems. Diseases can be caused by the most different reasons. This includes various injuries, for example, burns from hot food, dehydration, decreased immunity, lack of important vitamins and microelements, allergies, infectious components, tartar, poor oral care.
Of all the numerous diseases that can form in the mouth, infectious-inflammatory, fungal and viral, and dental diseases should be distinguished, dividing them into appropriate groups. In addition, there are a number of manifestations that are difficult to attribute to any of the listed groups. They will also be discussed below.
As you know, any disease has its own characteristic symptoms. This helps to decide not only on the choice of a specialist, but also to find out which pathology can be cured yourself, and which only with a specialist. Below are some of the most known diseases oral cavity.
Viral diseases
Human papilloma and herpes viruses can cause the formation of these pathologies in the patient’s oral cavity
Herpes. It is considered one of the most common diseases. Research shows that about ninety percent of people are infected with this virus. Often it is localized in the body, taking on a latent form. If the patient’s immune defense functions well, then herpes in most cases manifests itself as a small pimple that resolves without outside intervention. short term, which is usually no more than seven to ten days. When the immune system is weakened, the disease takes on more serious forms.
While at rest, the disease begins to take an active form with the following provoking factors:
- stress;
- cold;
- non-compliance with sleep patterns, lack of sleep,
- climatic: in cold, windy weather;
- menstruation,
- surgical interventions,
- immunosuppression.
The process of disease development occurs in stages and usually includes six stages. The first signs that make themselves felt are characterized by itching on the lips and slight tingling in this area. Then the lips become swollen, reddish and pain appears, which interferes with eating and talking. The next stage is characterized by the appearance of separate small bubbles or entire groups of them. After some time, the blisters begin to burst, turning into tiny ulcers. They have a hard crust coating that often cracks. The final stage is the gradual passage of ulcers and the disappearance of redness, as well as pain.
If the first symptoms of herpes are detected, you need to apply something cold, preferably a piece of ice, to your lips. And also treat with a high-quality balm to moisturize. The small bubbles that subsequently form must be lubricated with an ointment intended for this, which can always be purchased at any point in the pharmacy chain. For example, penciclovir helps. If the patient is frequently susceptible to exacerbations of this disease (on the recommendation of a doctor), antiviral drugs can be taken.
Papilloma. This renowned education may, caused by the papilloma virus, form on different areas bodies. There are several types of viruses, but one of them (human papillomas) can cause the manifestation of the disease in the oral cavity. There, these formations resemble white plaques in appearance. Papillomas may present serious danger, especially when it spreads to the throat area, when the patient has problems not only with hoarseness, but also with breathing. Besides this type The virus cannot be completely cured, you can only eliminate the clinical manifestations using one of the following methods:
- surgical intervention;
- chemically;
- cytostatic;
- the use of immunotherapy.
However, the possibility of combining the above methods is not excluded.
Infectious and inflammatory diseases
Diseases of this nature are a very common reason for patients to turn to various types of specialists - therapists, dentists or otolaryngologists. The most common infectious and inflammatory diseases will be discussed next.
Pharyngitis. Characterized by inflammation of the pharyngeal mucosa and, in particular, the throat. The disease is usually accompanied by soreness, a feeling of discomfort when eating and acute pain in the throat area.
Acute pharyngitis. There are many reasons for its manifestation. The development of the process can be triggered by cold or polluted air that the patient inhales, tobacco smoke, and various chemicals. In addition, the development of pharyngitis can also be affected by the presence of pneumococcal infection. In addition to those mentioned common features pharyngitis, you can also name such as general weakness, increase in body temperature, while its increase is noted only in acute case. This symptom is not typical for the chronic form.
As a rule, the diagnosis of this disease is carried out by a general examination by a specialist and taking a swab from the throat. Experts prescribe treatment of pharyngitis with antibiotics only in exceptional cases when the disease has complex nature currents. Basically, it is sufficient for the patient to follow a certain diet and take hot foot baths. Warm compresses on the neck, inhalations and warm milk with honey are excellent in overcoming the disease.
Glossitis. This disease is characterized by an inflammatory process, as a result of which the structure and color of the tongue changes. The provoking factors in most cases are oral infections. Various other causes can also affect the manifestation of the disease, for example, a burn of the tongue, excessive drinking, or trauma to the oral cavity, since they are a kind of port of infection. In addition, often among the people who become ill with this disease are patients who abuse spicy foods and low-quality mouth fresheners. Of course, the risk of developing glossitis increases significantly in patients who do not follow basic hygiene rules, for example, using someone else’s teeth cleaning equipment.
Signs of the disease include a burning sensation and a feeling of discomfort. Then, after some time, the patient’s tongue takes on a pronounced red color, and the process of salivation is activated. After some time, signs of the disease will be dullness or complete absence of taste. At the same time, in some cases, taste sensations do not disappear, but become perverted.
In the absence of timely and high-quality treatment, the consequences can be the most severe, because the tongue can swell so much that it will be difficult for the patient not only to eat, but also to speak. In addition, growths can cover the entire tongue. As a rule, treatment for glossitis consists of taking medications, as well as following a special diet based on liquid food.
Stomatitis. When they talk about infectious diseases oral cavity, then the first thing they mean is stomatitis, which is the most common among them. The patient's body becomes infected different ways. This can happen, for example, as a result of a mechanical injury. When the infection enters the patient’s body, ulcers begin to form, which have signs unique to stomatitis. In most cases, they begin to form inside the cheeks and lips, spreading to the root of the tongue and under it. The characteristic of ulcers may be that they are shallow. They can be single and round with smooth edges, covered in the center with a film. In most cases, these formations are very painful.
When treating stomatitis, the patient must use special toothpastes and rinses. They should not contain sodium lauryl sulfate. For severe pain, it is recommended to use anesthetics. In addition there are special means, which help remove the film from the ulcers, which significantly reduces the treatment time. This disease also involves the use of anti-infection medications prescribed by the doctor.
Herpes and stomatitis: what is the difference
Often, even doctors cannot immediately distinguish stomatitis from viral herpes; as a result of the infection, painful ulcers form in the patient’s mouth. Currently, the distinction is made based on some essential features characteristic of this particular pathology:
- if stomatitis is constantly localized in new areas, then herpes does not tend to choose other affected areas, appearing in the same place;
- stomatitis in most cases is localized on soft tissues, while herpes, as a rule, affects tissue areas adjacent to bone structures;
- with herpes, the manifestation of ulcers begins after the bursting of small blisters; with stomatitis, the inflammatory process begins with the formation of ulcers.
Gingivitis. This pathology is an inflammation of the mucous membrane of the gums. Happens quite often. This is a disease that affects women during pregnancy and adolescent patients to a greater extent.
Currently, gingivitis is divided into four types:
- catarrhal The most characteristic signs are bleeding with swelling and redness of the gums, itching;
- ulcerative-necrotic. It is characterized by the appearance of ulcers and necrosis on the gums. Also distinctive features symptoms inherent in this type of gingivitis are such as the presence of bad breath, acute pain, and enlarged lymph nodes. In addition, the patient experiences general malaise and a rise in temperature;
- hypertrophic. With this type of disease, you can observe an increase in the gum papillae, which cover some area of the tooth, and there may also be mild bleeding of the gums and slight pain;
- atrophic. It is characterized, as a rule, by the fact that the patient has an acute reaction to cold and hot food, while there is a decrease in the level of the gums and exposure of part of the tooth.
Treatment of gingivitis in the early stages can be painless and quick if the patient follows all the doctor’s oral hygiene instructions. Sometimes curettage is required. The doctor will remove plaque either closed, using special instruments, or open, cutting the gums.
In case of gingivitis of an infectious-inflammatory nature, the first step is to eliminate the causative agent of the infection. Antibacterial or antifungal agents are prescribed here. The chronic form of the disease requires treatment of the oral cavity with sodium bicarbonate solution, as well as anti-inflammatory drugs.
The presence of gingivitis often indicates a weakened immune system in the patient. In this regard, it is necessary to treat not only the inflammatory process, but also to increase the body's defenses. Drugs from the group of immunocorrectors will help with this.
Fungal diseases
Research has found that almost fifty percent of the world's population are passive carriers of Candida fungus. It can become active under favorable conditions, especially when the patient’s immune system is weakened. There are several types of candidiasis:
Thrush. The most common type. It is characterized, as a rule, by a white coating and dryness of the cheeks and lips from the inside, as well as on the back of the tongue and palate. These symptoms may be accompanied by a feeling of discomfort and burning, while young patients cope with thrush much easier than adults.
Atrophic. This type is considered to be the most painful. As the disease develops, the mucous membrane becomes dry and the oral cavity becomes bright red. Hyperplastic candidiasis is characterized by a large layer of plaque; if an attempt is made to remove it, it ends in bleeding of the surface. In most cases, this type of fungal disease is caused by wearing a plate prosthesis for a long time, resulting in drying out of the mucous membrane of the tongue, palate and corners of the mouth with further development inflammatory process. For proper treatment of candidiasis, it is necessary to accurately determine its type, and this is only possible by conducting a whole range of tests.
Lichen planus. Also a fairly common type of fungal disease. It is characterized by the formation of ulcers, plaques and blisters and redness in the patient’s mouth. Quite often, lichen can be combined with gastric and liver disorders, diabetes.
Other diseases
In addition to the diseases that were mentioned above, there are a number of such diseases that hardly belong to one or another group. An example is the disease of the so-called geographic tongue. This, as a rule, is not a dangerous pathology of the tongue, and it is difficult to call it a disease. It is characterized by grooves covering the tongue, which are somewhat similar to a geographical map.
However, among the diseases that cannot be classified, there are also those that need attention. One of these ailments is oral dysbiosis. The factors that cause the development of the disease in most cases are the use of antiseptics and antibiotics to eliminate other causes during treatment.
The presence of dysbacteriosis may be indicated by minor cracks in the corners of the lips, as well as loose teeth with damage to the enamel. To combat dysbiosis, you need to restore the microflora of the oral mucosa.
Xerostomia. This disease is characterized by dryness, burning and inflammation of the oral mucosa. The reason for this is a disruption in the functioning of the mucous and salivary glands, as a result of which the secretion of mucus and saliva is reduced. In most cases, the disease manifests itself in patients who suffer from allergies, diabetes, and some other pathologies. Treatment is based on eliminating provoking factors. In addition, the necessary sanitation of the oral cavity is carried out.
Dental diseases
Periodontal disease. As a result of the inflammatory process, dystrophy of all periodontal tissues is formed. Characteristic features is anemic gums, you can notice not only the necks, but the tooth roots. Tooth displacement and mobility are noted. In this case, patients do not experience pain. All this affects timely contact with a specialist, since the disease often has an unnoticeable course. Which ultimately leads to the development of the following disease, which is discussed below.
Periodontitis. It is characterized by inflammation of the tissues that surround the teeth, mainly the gums and bones. Patients over forty years of age suffer less from caries than from this disease. And among those who have reached the age of sixty-five, according to studies, almost 80 percent develop this disease. It has been noted that men are less likely to suffer from periodontitis than women. The first symptom of the disease is gum bleeding, which can be observed both during brushing and eating. Further symptoms may be accompanied by gum swelling, as well as sensitivity to both cold and hot foods.
The development of periodontitis in most cases is influenced by malocclusion, as a result of which a separate group of teeth experiences overload. By the way, more than 60 percent of the population suffers from this pathology. As the patient ages, systemic diseases can act as provoking factors, for example, in men it is ischemia, diabetes. The weaker half has hormonal imbalances during menopause and various problems associated with the thyroid gland.
During treatment, first of all, it is necessary to take measures to remove plaque and dental deposits. Then treat the gums medicines which relieve inflammation. In almost one hundred percent of cases, antibiotics are used to treat this disease. Patients are often prescribed physical procedures, for example, involving a laser, which affects the inflammatory focus.
Surgical intervention is also practiced, especially in cases where tooth mobility occurs and there is severe inflammation and tooth mobility. Thanks to them, it becomes possible to clean dental deposits in hard-to-reach areas under the gums. For the purpose of prevention, it is necessary to take measures to correct the bite and try to avoid complications of chronic diseases that can provoke the development of periodontitis.
As mentioned at the beginning, these are only the most common diseases. There are quite a lot of them. Some inflammations are not very complex in nature, while others, on the contrary, pose a serious threat. The main thing is to identify the disease in time and take measures to treat it.
Finally
Oral disease is a kind of mirror that reflects problems occurring within the entire body. The development of the disease can be triggered by gastrointestinal disorders, various types of anemia and lack of vitamins in the body, weakened immunity, endocrine problems, allergies, and often more serious diseases. In this regard, experts advise not to delay visiting a doctor if you suddenly discover the presence of ulcers, blisters or redness in the oral cavity, regardless of whether they are painful or not. This is the only way to hope for quick and effective treatment.





