The problem of diseases of the oral cavity is now quite relevant. After all, everyone wants to have beautiful and healthy teeth. But not many can boast of a Hollywood smile. And the problems are not even in the teeth themselves, but in the symptoms that accompany oral diseases.
In the early stages, they may not manifest themselves, in later cases, the process of destruction and loss of teeth already begins.
To protect yourself from various diseases, you should regularly visit the dentist's office. Only in this case, the disease can be recognized at its very beginning and the development and consequences can be prevented.
Diseases of the oral cavity
The most common diseases oral cavity in adults are considered: stomatitis, glossitis, gingivitis.
Stomatitis
Stomatitis is a lesion of the oral mucosa. Often stomatitis is provoked by various mechanical injuries, for example, after a bite of soft tissues or a cut on the sharp edge of a tooth. Usually, such injuries heal quickly, but in some cases they lead to complications and the development of stomatitis.
Not infrequently, toothpastes containing sodium lauryl sulfate are the cause of the onset of the disease. Stress and insufficient intake of vitamins are another reason why stomatitis develops.
In some cases, the disease provokes allergic reactions. For example, food or medicines.
Recently, it has been suggested that stomatitis can be inherited. If someone in the family suffered from this disease, then there is a high probability that it will be passed on to another generation.
Symptoms of stomatitis
With a disease on the oral mucosa, small sores can be found. At an early stage, there is a slight redness, which sometimes swells and causes discomfort in the form of a burning sensation. Gradually, this leads to the formation of ulcers.
Treatment of stomatitis
Treatment is aimed primarily at eliminating the cause of stomatitis. If you feel pain, your doctor may prescribe anesthetics. It is not uncommon to use antiviral drugs, as well as agents that help rapid regeneration.
Glossitis
Glossitis is a pathological condition in which the tongue is affected. Most often, the disease affects men. With glossitis, pains appear in the tongue when eating, talking. It changes color, is sharply hyperemic and coated with a coating. There is a smell from the mouth and erosion, which can bleed.
Causes of glossitis
The causes of glossitis can be:
- Viruses;
- Bactria;
- Injuries;
- Fungi.
Glossitis treatment
Treatment of glossitis is based on the treatment of the oral cavity, several times a day. You can rinse your mouth with a solution of furacilin or chlorhexidine.
Gingivitis
Gingivitis is called inflammatory process gums This disease can be found in pregnant women and adolescents. There are many reasons why gingivitis develops.
For example, a lack of vitamins, an erupting tooth, diseases of the gastrointestinal tract or a decrease in immunity.
Very often, burns of the oral mucosa, infections, food debris, and smoking can lead to gingivitis.
Symptoms of gingivitis
There are several types of gingivitis and each of them will have its own symptoms.
- Catarrhal is characterized by redness, bleeding and swelling.
- Ulcerative-necrotic speaks for itself. Ulcers appear on the oral mucosa, bad breath, body temperature rises to 39 degrees.
- Hypertrophic is characterized by an increase in gingival papillae that cover part of the tooth. They are painful and bleed.
- Atrophic means atrophy of the gum tissue. In this case, the patient complains of pain when taking cold or hot food.
Treatment is based on rinsing the mouth with various solutions. You should also identify the cause of the appearance of gingivitis, and then only begin the appropriate treatment.
In addition to the diseases described above, one should be very careful about.
Oral diseases can cause various reasons. These are dental problems and diseases. internal organs, and damage (for example, hot or spicy food), and general dehydration, vitamin deficiency, as well as many other factors. All diseases that can occur in the human mouth can be divided into viral, infectious-inflammatory and fungal diseases. In addition, there are several unpleasant sores that cannot be attributed to any of these groups. In order to correctly choose a specialist to whom you need to contact with a particular problem, as well as in order to know which disease you can treat yourself and how, and which one cannot, you need to know each of the diseases of the mouth “by sight”.
Viral diseases
Viral diseases in the human oral cavity can cause herpes virus and human papillomavirus.
Herpes is one of the most common diseases. It is believed that ninety percent of people are infected with this virus.
An example of herpes on the lips.
Often this virus is located in the body in a latent form. In a strong person, it can manifest itself only as a small pimple on the lip, dying off without outside help within one to two weeks, while in a weakened person, herpes manifests itself much more significantly.
Calm herpes can be triggered "to action" by factors such as stress, surgery, colds, fever, lack of sleep, wind, cold, menstruation, immunosuppression.
Herpes develops, as a rule, in stages, passing through six stages. It all starts with itching and tingling on the lips and adjacent tissues, after which the lips swell, redden, soreness appears that interferes with eating and speaking, followed by the appearance of single vesicles or entire groups with vesicles. After a while, the blisters burst and turn into small ulcers. Ulcers are covered with a hard crust that can crack. In the final stage, the ulcers gradually disappear, redness and pain disappear.
At the first symptoms of herpes, ice should be applied to the lips and moistened with special balms. The bubbles that appear are lubricated with a special ointment that can be bought at a pharmacy without a prescription (for example, Penciclovir or Abreva). If a person is prone to too frequent exacerbations of herpes, then the doctor may prescribe antiviral drugs for him.
Papilloma
Papilloma in humans can occur in various parts of the body, but one type of human papillomavirus can cause the appearance of papillomas in the oral cavity. In the mouth, these sores look like cauliflower, that is, white plaques appear.
The most unpleasant consequences of this disease occur when it gets to the throat, because it can cause not only hoarseness, but also difficulty breathing.
Unfortunately, it is impossible to completely cure the human papillomavirus, so the treatment consists in eliminating the clinical manifestations. If we talk about the treatment of this virus in in general terms, then it comes down to choosing one of the methods: surgical, chemical, cytostatic, immunotherapy, or a combination of the above methods.
Infectious and inflammatory diseases
Infectious diseases of the oral cavity are the most common problem for which people turn to dentists, otolaryngologists or therapists. This species includes pharyngitis, gingivitis and.
Pharyngitis is an inflammation of the mucous membrane of the pharynx and, in particular, the throat. As a rule, it is accompanied by perspiration, discomfort and severe sore throat.

Acute pharyngitis.
Pharyngitis can provoke various factors: inhalation of cold or polluted air, tobacco smoke, various chemical pollutants. In addition, pharyngitis can also be caused by an infection (pneumococcus).
To the symptoms of pharyngitis already listed above (discomfort, sore throat and sore throat), you can also add general malaise, fever (the latter is typical only for acute pharyngitis, but not for chronic).
Diagnosed this disease general examination and throat swab. Doctors treat pharyngitis with antibiotics only in difficult cases, as a rule, only a special diet, hot foot baths, warm compresses on the neck, warm milk with honey, inhalations and rinses are enough.
Glossitis
Glossitis is an inflammatory process. It changes the structure as well as the color of the language. It is caused by oral infections. Glossitis can be provoked by a burn of the tongue, excessive love for hot drinks, injuries of the oral cavity and tongue, because all this is a kind of “pass” for infection. In addition, those who abuse alcohol, spicy foods and mouth fresheners are at risk. Of course, the chances of getting glossitis are also increased for those who neglect oral hygiene, in particular, use other people's toothbrushes.
The first symptoms of the disease are burning, discomfort, a little later, the color of the tongue becomes bright red, salivation increases. Further symptoms are dullness (or complete absence) of taste sensations. Although it is noticed that sometimes the sensation of tastes does not disappear, but is perverted.
If there is no treatment for this infection, the swelling of the tongue reaches such proportions that it becomes very difficult for a person to speak and eat, in addition, the tongue itself becomes covered with growths.
Treatment of glossitis is prescribed by a dentist. It consists in taking medications and a special diet based on semi-liquid food.
Gingivitis is characterized by inflammation of the lining of the gums. This is a fairly common disease that adolescents and pregnant women are most susceptible to.

Gingivitis affects the gums.
There are four types of this disease: catarrhal gingivitis, ulcerative necrotic, hypertrophic, atrophic.
- catarrhal gingivitis is characterized by symptoms such as redness and swelling of the gums, their itching and bleeding;
- with ulcerative necrotic gingivitis, ulcers and necrotic areas appear on the gums, in addition, the symptoms characteristic of this disease are bad breath, severe soreness, general weakness, fever and swollen lymph nodes;
- hypertrophic gingivitis enlarges the gingival papillae and covers part of the tooth with them, in addition, slight bleeding of the gums and mild soreness are possible;
- with atrophic gingivitis, a person begins to react sharply to hot and cold, the gum level decreases, and the tooth is exposed.
A dentist can treat gingivitis quickly and painlessly if treated early, and will also give oral hygiene advice to avoid this disease in the future.
Stomatitis
If we talk about infectious diseases of the oral cavity, then the most common of them is stomatitis.
Possible infection in the body different ways e.g. due to mechanical injury. After infection, a person develops special ulcers that are characteristic only for stomatitis. They are localized in inner surface cheeks and lips, at the root of the tongue, as well as under it. Have ulcers next view: shallow, single, round, smooth edges, and the center is covered with a film, as a rule, ulcers are very painful.
In the treatment of this disease, it is necessary to use special toothpastes and mouth rinses that do not contain sodium lauryl sulfate. To relieve the soreness of ulcers, anesthetics should be used. In addition, there are special drugs that help remove the harmful film from ulcers, which speeds up the treatment. And, of course, you can not do without anti-infection agents that the doctor will prescribe for you.
How to distinguish herpes from stomatitis?
Sometimes it is very easy to confuse the viral one that caused the infections, because in both cases painful wounds appear in the person's mouth. There are three characteristic differences between these diseases:
- herpes always appears in the same place, stomatitis always chooses new affected areas;
- herpes always affects those areas of tissue that are adjacent to the bones, stomatitis “likes” soft tissues more;
- during herpes, ulcers appear due to the bursting of small bubbles, and stomatitis initially begins with ulcers.
fungal diseases
Half the population the globe are inactive carriers of the Candida fungus. It can be activated if the body's immune defenses are weakened. Candidiasis (a disease caused by Candida) is of several types.
The most common is thrush. Its symptoms are dryness and white coating inside the cheeks and lips, on the palate and back of the tongue. All this is accompanied by a burning sensation and severe discomfort, and children tolerate thrush much easier than adults.
Most painful appearance candidiasis - atrophic. The mucous membrane of the oral cavity acquires a bright red color, becomes dry. With hyperplastic candidiasis, a thick layer of plaque appears, when you try to remove it, the surface begins to bleed.
This kind fungal disease, as atrophic candidiasis usually provokes prolonged wearing of lamellar prostheses. The mucous membrane of the tongue, palate and corners of the mouth dries up and becomes inflamed.
Treatment of the disease "candidiasis" can only be prescribed by a doctor, because it is extremely important to correctly determine its type, and for this you need to conduct a whole series of tests.
Lichen planus is another type of fungal disease. It causes plaques, blisters, ulcers and redness in a person's mouth. As a rule, lichen is combined with diseases such as diabetes, diseases of the stomach and liver.
Other diseases
In addition to the above diseases, there are several that are difficult to attribute to one or another group. For example, a geographical language, a completely harmless disease (although it is difficult to call it a disease, rather a change) of the language. In this case, the tongue is covered with a kind of grooves resembling geographical map.
But among the unclassified diseases, there is one that is still worth paying attention to - this is oral dysbacteriosis. The cause of this disease is the intake of various antibiotics, antiseptics during the treatment of other problems.
Symptoms of dysbacteriosis begin with minor ones - cracks in the corners of the lips, bad smell from the mouth and reach the loosening of the teeth and damage to their enamel. To overcome dysbacteriosis, it is necessary to restore the healthy microflora of the oral mucosa.
What are diseases of the oral mucosa?
Diseases of the oral mucosa (stomatitis) are a fairly common problem. But their correct diagnosis is complicated by the fact that many diseases of the oral cavity occur with similar or even the same symptoms.
Stomatitis is a wide range of different diseases of the tongue, lips or palate. Accordingly, they are called glossitis, cheilitis and palatinitis. When the mucous membrane of the mouth thickens, becomes horny and peels off, they speak of a special type of disease - leukoplakia.
Causes of diseases of the oral mucosa
The reasons why the oral mucosa is exposed to stomatitis are diseases of the gastrointestinal tract, cardiovascular problems, a decrease in the body's immune forces, metabolic disorders and factors that directly affect the oral mucosa.
Stomatitis can also occur due to various dental reasons. For example, diseases often develop due to a person’s non-compliance with the rules of hygiene and oral care, decayed teeth and dental deposits play their role. Violations of the technique of dental procedures can also cause stomatitis, since dissimilar metals and chemical substances in the treatment of teeth and prosthetics, they can create microtraumas.
Symptoms of diseases of the oral mucosa

Symptoms of diseases of the oral mucosa are directly dependent on the type of stomatitis.
Catarrhal stomatitis among diseases of the oral mucosa is the most common. It is caused by local factors, which include poor oral care, dental plaque and disease, oral dysbacteriosis and all kinds of pathological processes of the gastrointestinal tract (gastritis, duodenitis). When catarrhal stomatitis is caused by helminthic invasion, the mucous membrane of the mouth swells, becomes covered with white or yellow coating and becomes painful. The patient has noted increased salivation, gums may bleed, an unpleasant odor appears from the mouth.
Ulcerative stomatitis- a fairly serious disease of the oral mucosa. It develops both independently and as a complication of catarrhal stomatitis. Often this disease occurs in people suffering from a stomach ulcer or a chronic form of enteritis. The risk group also includes people suffering from infectious and cardiovascular diseases, blood diseases and poisoning. Ulcerative stomatitis affects not only the upper layer of the oral mucosa, but also its entire thickness. The initial symptoms resemble catarrhal stomatitis, but after a while they appear characteristics ulcerative lesions of the mucous membrane: body temperature rises to 37.5 degrees, the patient feels weakness, headache; lymph nodes may become enlarged and painful. eating is difficult due to severe pain.
Aphthous manifests itself with the appearance of aphthae (sores) on the mucous membrane of the mouth. Aphthae can be oval or round, red at the edges and greyish-yellow in the center. Aphthous stomatitis develops mainly due to diseases of the gastrointestinal tract, allergic reactions. Viral infections or rheumatism can also be causes. In addition to damage to the oral mucosa and its soreness, there is a general malaise, the patient's body temperature rises, and so on.
Found a mistake in the text? Select it and a few more words, press Ctrl + Enter
Leukoplakia is a chronic lesion of the oral mucosa, which is based on increased keratinization of the epithelium (hyperkeratosis). It affects mainly men after 40 years and is localized on the mucous membrane of the cheek, in the corners of the mouth and on the lateral surfaces of the tongue. The causes of leukoplakia can be mechanical injuries of the mucous membrane: cuts with hooks from a denture, burns from hot or spicy food, and so on. This disease most often does not have pronounced symptoms, only sometimes the patient may feel slight itching and burning. But the danger of the disease lies in the fact that it can turn into malignant forms, so the patient needs to consult an oncologist.
Treatment of diseases of the oral mucosa
The basis for the treatment of diseases of the oral mucosa is the elimination of the causes that provoked them. The oral cavity is subject to sanitation, the sharp edges of the teeth are treated, and the denture is properly adjusted. The patient is advised to stop smoking and eating spicy and hot foods.
Tartar with stomatitis is removed, and the teeth are to be treated. It is necessary to rinse the oral mucosa with antiseptic agents (chlorhexidine or aminocaproic acid solutions). Also apply folk remedies: infusions and decoctions of chamomile and calendula. If signs of stomatitis persist after 5-10 days, most likely they were caused by a disease of the gastrointestinal tract or helminthic invasion. Then local treatment is combined with the general one.
stomatitis are called inflammatory diseases of the oral mucosa. There are stomatitis with different localization of the inflammatory process. In case of damage to the mucous membrane of only the tongue, they speak of glossitis, of the gums - of gingivitis, of the lips - of cheilitis, of the palate - of palatinitis.
The most common form of damage to the oral mucosa is inflammation of the gums - gingivitis. It occurs under the influence of mechanical irritation, as a result of deposition on the necks of the teeth significant amount tartar, industrial dust, as well as periodontal disease (alveolar pyorrhea). In addition, gingivitis can occur with hypo- and avitaminosis, in particular with avitaminosis C (scorbutic gingivitis). You can meet with the so-called hypertrophic gingivitis that occurs during pregnancy and during puberty.
There are traumatic, symptomatic, infectious and specific stomatitis. The cause of traumatic stomatitis can be mechanical trauma, chemical damage to the oral mucosa, etc.
Symptomatic stomatitis is the result of a general disease (gastrointestinal tract, cardiovascular system, blood).
Infectious stomatitis occurs with measles, scarlet fever, diphtheria, malaria, etc.
Specific stomatitis is the result of lesions of the oral mucosa with syphilis, tuberculosis, and fungal diseases.
Catarrhal stomatitis
Limited damage to the mucous membrane of the gingival margin - catarrhal, or serous, gingivitis - occurs in the absence of a systematic proper care behind the oral cavity, with insufficient chewing of solid foods, especially vegetables and fruits. Inadequate natural self-cleaning of teeth favors the rapid deposition of tartar, which in turn increases inflammation of the gums. Incorrectly and closely spaced teeth, forming niches, create conditions conducive to the deposition of tartar in them and the development of gingivitis. Chewing food with the teeth of only one right or left side due to dental disease or other causes also contributes to increased deposition of tartar on the teeth that are not involved in the processing of food, and causes unilateral inflammation of the gums.
The factors of mechanical irritation of the gums that cause catarrhal inflammation include sharp edges of the roots of the teeth, incorrectly applied fillings in the area of the gum margin, removable and non-removable dentures that do not adhere well to the neck of the tooth.
Some professions play a certain role in the development of gingivitis. Workers in cement factories, flour mills, masons, grinders of glass and mother-of-pearl, workers in foundries harmful effect exerts mechanical irritation with the dust of these industries. In case of insufficient ventilation of the working room, especially a lot of industrial dust accumulates. Once in the mouth, it lingers at the gingival margin and causes inflammation of the gums. It is manifested by a wide red stripe stretching parallel to the gingival margin along the entire dentition. It also extends to the gingival papillae. Gingivitis is usually most pronounced in the region of the anterior teeth (Fig. 54). Gradually, the gingival margin and gingival papillae increase, become painful, hyperemic, and bleed easily when touched and brushed. In the future, the gum surrounds, as it were, a shaft of the neck of the teeth or roots, forming pockets in which there is not only tartar, but often a yellowish purulent mass containing in large numbers microbes. In the most severe cases, due to the spread of the inflammatory process to the ligament of the tooth and its destruction, the teeth become mobile. At the beginning of the disease, there is a slight pain of a aching nature. Later, patients complain of severe pain. Bleeding increases, food intake is difficult, it is necessary to limit yourself to softer, liquid food that does not require chewing.
Catarrhal stomatitis of other parts of the oral mucosa most often accompanies general diseases, but can also manifest itself. It occurs as a complication of catarrh of the upper respiratory tract, gastrointestinal and infectious diseases. More often than others, children suffer from catarrhal stomatitis, especially infants - weakened, suffering from dyspepsia, artificially fed. A common cause of the disease is the use of dirty nipples and toys.
The causes of serous inflammation of the oral mucosa can be irritation with hot or very cold food or water, the abuse of salty, sour foods, alcohol, tobacco, and in some individuals, the use of drugs (iodine, bromine, antibiotics, sulfanilamide drugs, etc.) .). The cause of inflammation can be irritation of the denture if it does not fit well to the mucous membrane of the palate or gums, or if it is not kept clean enough. The process can be localized in a limited area or spread to the entire surface of the oral cavity - lips, cheeks, gums, palate, tongue. The disease manifests itself in the form of more or less severe hyperemia of various parts of the oral mucosa. In the future, swelling of these areas also appears. The temperature, especially in children, may be elevated. Usually a few days after the cessation of irritation, recovery occurs. In weakened individuals, the process often turns into ulcerative stomatitis.
Catarrhal stomatitis occurs with many infectious diseases. In each case, its manifestations are different. With measles, even before the appearance of a characteristic rash on the skin and inflammation of the mucous membranes of the nasopharynx and eyes, white dots form on the mucous membrane of the cheeks near the corners of the mouth, somewhat rising above the level of the mucous membrane. Bright red, shiny spots form around them. irregular shape. These are the so-called Filatov-Koplik spots (Filatov-Koplik symptom), which are characteristic only of measles. Recognition of these spots allows early diagnosis of measles and timely isolation of a sick child.
With scarlet fever, even before the appearance of a skin rash on the mucous membrane of the tongue and in the throat, characteristic early signs. The tonsils, palatine arches and uvula turn bright red and appear swollen - the so-called scarlatinal angina. The tongue is covered with a grayish coating. Already during this period, the child becomes dangerous to others. On the 3-4th day from the onset of the disease, the tongue begins to be freed from plaque, and after another 1-2 days it becomes intensely red. Reddened papillae sharply protrude on it, giving its surface a resemblance to raspberries. Therefore, the language of persons with scarlet fever was called "raspberry". By the 10th day from the onset of the disease, the tongue becomes smooth, as if varnished, and by the 12-15th day it takes on its usual appearance.
With certain forms of influenza, especially viral, catarrhal stomatitis may also occur in combination with areas of hemorrhage. Their appearance is associated with a sharp hyperemia of blood vessels and areas of petechial hemorrhages. Usually these manifestations disappear by the end of the 2nd week of the disease. Serous stomatitis also affects patients with diphtheria, pneumonia, typhoid, dysentery, etc.
This disease refers to chronically occurring inflammatory processes. It is observed most often in pregnant women, as well as during puberty in boys and girls (Fig. 55). Hypertrophic gingivitis is characterized in the initial stage by swelling of the gums, which acquire a bluish-red color. In the future, there is an overgrowth of the gums and papillae, which can partially or completely cover the crowns of the teeth on the upper and lower jaws at the same time. The anterior teeth are most commonly affected. The overgrown gum forms deep gum pockets. When examining pockets, they can detect food debris, mucus, deposits of tartar, etc. Continuing to grow, the gum begins to disturb the patient: it bleeds and becomes painful.

Ulcerative stomatitis
Ulcerative stomatitis is observed more often in persons with reduced nutrition or malnourished general severe diseases. The main reason should be recognized as a decrease in the resistance of the whole organism. In some cases, it is a consequence of advanced catarrhal gingivitis. Ulcerative stomatitis can occur with various common infectious diseases, blood diseases, poisoning with lead, mercury, bismuth, etc. The disease begins with minor signs of inflammation: redness, slight swelling and bleeding of the mucous membrane, burning sensation. When localized on the gums, the ulcerative lesion is especially noticeable in the area of the interdental papillae, which seem to be cut off with a knife. In the initial stage of the process, the mucous membrane is littered with small purulent vesicles that burst and lead to the formation of ulcers with pointed, uneven edges. The surface of the ulcer is usually covered with a yellowish film.
The tongue and lips are rarely affected by the ulcerative process. Only signs of serous inflammation can be noted here. In the future, the process, progressing, captures the mucous membrane of the tonsils. Patients complain of pain, especially when eating, as well as bleeding gums and bad breath. Due to difficulty in eating, the patients become weak. Often headaches and sleep disturbance. The submandibular lymph nodes react to the inflammatory process: they are enlarged and painful. The temperature can rise up to 38°C. Saliva becomes viscous. In the blood - leukocytosis, increased ESR.
Stomatitis arising from the use of drugs
Some drugs are not well tolerated by some patients and may side effect. One of the pronounced symptoms of drug intolerance is inflammation of the oral mucosa. Sometimes it is combined with rashes on the skin of the trunk and limbs. Most often, such manifestations occur in patients who have received sulfa drugs or antibiotics for a long period, primarily penicillin, streptomycin, biomycin or chloramphenicol. Some drugs play the role of allergens in such cases, and the reaction can occur only after a few (3-7) days after taking the drug.
Some drugs cause only dry mouth, others - phenomena on the oral mucosa, resembling serous stomatitis. Most often, such changes in the oral mucosa occur when taking antibiotics by mouth or when rinsing the mouth with antibiotic solutions.
Stomatitis can also occur with the use of sulfa drugs. In these cases, they often have the character of cystic eruptions, which capture not only the mucous membrane, but also skin. Sometimes the temperature can rise to 38°C. There is a headache, general weakness. Catarrhal or even ulcerative stomatitis develops on the mucous membrane of the oral cavity, erosion that does not heal for a long time. Rashes on the skin in this case usually have a polymorphic character.
Medicinal stomatitis with individual intolerance can also occur during treatment with iodine, bromine, arsenic, antipyrine group, barbiturates, etc.
Aphthous stomatitis
There are acute aphthous stomatitis and chronic recurrent aphthous stomatitis.
Infection. More common in children younger age, although in some cases it also affects adults. The most prone to this disease are children suffering from diathesis. A. I. Rybakov considers one of possible causes its occurrence is damage to the large intestine. There is no complete clarity in the etiology of the disease. This disease can be passed from one child to another. If elementary sanitary and hygienic rules are not observed, entire groups of children in nurseries or kindergartens can be affected.
The disease is acute, high temperature and bad general well-being. Eating is sharply hampered due to damage to the oral mucosa. There is profuse salivation, bad breath. Regional lymph nodes are enlarged and their palpation is painful.
Numerous aphthae (vesicles that quickly form erosion, even an ulcer) appear on the oral mucosa. They are localized on the mucous membrane of the lips, cheeks, palate (Fig. 56). The disease usually lasts up to 2 weeks and ends with recovery. We observed acute aphthous stomatitis in both children and adults with viral influenza.

Chronic recurrent aphthous stomatitis more common in adults. Its reasons have not yet been elucidated. Many authors, including A. I. Rybakov, note the seasonal nature of the lesion with aphthous stomatitis. According to our data, chronic recurrent aphthous stomatitis most often occurs in the spring-autumn period.
Clinical manifestations of the disease are characteristic. Usually, on the mucous membrane of the lips, cheeks, palate or tongue, several small, very painful round or oval aphthae appear with a small bright red rim (Fig. 57). The cycle of development of each aphthae usually lasts 8-12 days, and while some aphthae heal, new ones appear. The appearance of aphthae is accompanied by soreness, especially when they are localized on the tongue. After complete healing, the rash may reappear. The disease has been going on for years.

Thrush
Thrush belongs to the group of fungal diseases. Usually affects infants and children early age. The most common route of spread is dirty objects (nipples, toys, etc.).
Pearly white plaques form on the bright red mucous membrane of the tongue, cheeks, and palate. Gradually increasing, the plaques merge with each other. The mucous membrane is covered with a grayish coating. In severe cases, the fungus spreads to the tonsils, pharynx, and even the esophagus. Often the child refuses to eat, the general condition can be severe.
Occupational lesions of the oral mucosa
Studies have shown that workers in some industries may experience specific changes in the oral mucosa.
Mercury stomatitis. Occupational disease occurs in workers of some industries (mirror factories, factories for the manufacture of thermometers, some fur enterprises, etc.), as well as in the treatment of mercury preparations. Intoxication can quickly cause the phenomena of stomatitis.
Patients complain of the taste of metal in the mouth. Then the phenomena of irritation and inflammation of the gums in the region of the molars and lower incisors, and subsequently in other groups of teeth, join. The gums become bluish in color, loosened, bleed easily, erosions, ulcers are formed.
In severe cases, the lesion extends to the mucous membrane of the lips, palate, tonsils. With a pronounced necrotic process, destruction is possible bone tissue and tooth loss. Eating is difficult. Individual susceptibility to mercury has great importance in the development of this disease.
Preventive measures in the workplace include strict isolation of workers from the resulting mercury vapor, powerful supply and exhaust ventilation, and compliance with sanitary and hygienic working conditions. At least 2 times a year, workers must undergo a preventive examination by a dentist. Persons with chronic inflammatory diseases of the oral mucosa should not work in such industries.
Lead stomatitis. Occupational disease occurs among workers in printing houses (typesetters, printers), lead mines, painters who deal with lead paints. Lead poisoning is most often chronic. On the free edge of the gums, congestive hyperemia and looseness appear with the formation of a dark border. The latter is the result of the deposition of lead sulfide on the mucous membrane. In the future, such deposits can form on the mucous membrane of the cheeks, lips and tongue. It should be emphasized that the presence of such a border does not necessarily indicate lead poisoning; it only shows that lead is deposited on the mucous membrane. With lead poisoning, profuse salivation, a metallic taste in the mouth, weakness, headaches, slow pulse, so-called lead colic and other characteristic symptoms appear.
Preventive measures are the same as for mercury poisoning.
Professional leukoplakia. Recent studies show that workers in some industries (associated with benzene compounds, with dry distillation of coal tar, with phenol and amino plastics, with the production of aniline dyes, etc.) may develop areas of thickening and keratinization of the oral mucosa. This disease is called leukoplakia.
Usually, workers do not complain and changes in the mucous membrane are first detected during preventive examinations by a dentist. The keratinization of the mucous membrane begins in the region of the corner of the mouth, later localizing on the cheeks along the line of closing of the teeth (Fig. 58). These changes are located symmetrically on the mucous membrane of the right and left cheeks. Only in individual cases lesions pass to the lip (in the corner of the mouth) or capture individual sections of the mucous membrane of the alveolar process (in the sky).

These changes are the result of trophic disorders that occur in the tissues of the oral cavity during chronic exposure to certain chemicals.
In addition to the usual recommended preventive measures, it is necessary that the workers of such workshops must be registered with the workshop dentist, since any kerato-like changes should be attributed to precancerous conditions.
Treatment of diseases of the mucous membrane
Patients with stomatitis are examined together with a therapist to determine the causes of the disease, if complex treatment is necessary. Treatment of stomatitis resulting from exposure to mechanical factors should begin with their elimination. The sharp edges of the teeth and dentures should be ground, incorrectly applied fillings and poorly made dentures should be replaced, and tartar should be removed. The intake of very cold or hot, salty and sour foods, alcohol, smoking is completely excluded. The mucous membrane is carefully treated with a 3% hydrogen peroxide solution. Assign frequent rinsing with a solution of potassium permanganate and baking soda.
Hexamethylentotramini aa........ 0.3
Glycerini q. s. M.f. emulsionis
D.S. For dental office
Among other therapeutic measures importance has a diet. Food should be non-irritating, liquid, nutritious, rich in vitamins and high in calories.
Infectious stomatitis, like other lesions of the oral mucosa, requires careful care of it. It is necessary to carry out regular irrigation with weak antiseptic solutions (potassium permanganate, furatsilin, etc.), lysozyme lotions.
When treating stomatitis caused by the action of various medicines, it is necessary first of all to stop taking these medicines. Diphenhydramine is recommended at 0.03 g 3 times a day, lubrication of the affected areas of the mucous membrane with nystatin ointment. Plentiful drink, vitamins B 1 and C are prescribed.
Aphthae with aphthous stomatitis are treated with methylene blue. Assign lysozyme rinses, sulfa drugs, antibiotics. AT last years a number of clinics treat chronic recurrent aphthous stomatitis with γ-globulin and cortisone.
Aerosol treatment with antibiotics gives good results.
With thrush, alkalization of the oral cavity is carried out by rinsing with 1-2% soda solution, 0.5% borax solution. General treatment should be aimed at increasing the body's resistance (the appointment of vitamins K, group B, C, etc.).
glossalgia
This disease is characterized by a violation of the sensitivity of the tongue. Women suffer more often (according to our data, in 90-92% of cases).
Although the etiology and pathogenesis of this disease have not been fully understood, it tends to be considered as a functional lesion related to language neuroses. Glossalgia often accompanies chronic diseases of the gastrointestinal tract (gastritis) and some blood diseases. In some cases, it also occurs in menopause. The cause of glossalgia may be local irritations of the physicochemical order - oxidizing prostheses made of dissimilar metals, the edges of destroyed teeth. The symptoms of this disease are very painful for patients - these are constant or often recurring pains, as well as itching and burning in the tongue (lateral surfaces, tip of the tongue). Patients are very irritable, suspicious, tearful, suffer from cancer fear (carcinophobia). During external examination, the tongue, as a rule, does not reveal pronounced pathological changes. In some cases, you can see small areas with hyperemic and painful papillae, in some places with minor cracks in the mucous membrane.
Patients with glossalgia should be carefully examined, since its manifestations may be the first symptom of general diseases, for example, some blood diseases.
An important place among the therapeutic measures for this disease is occupied by psychotherapy, because the removal of cancerophobia greatly facilitates further treatment patient and to some extent affects his success.
Each patient should undergo a thorough sanitation of the oral cavity, which is important element complex treatment of glossalgia.
The treatment is general therapy. Patients are prescribed multivitamins, vitamins B 12, 200 mcg in the form of injections (10 injections), 1% solution of nicotinic acid - 10 injections. Novocaine blockade (1%) for a course of 10-12 injections.
Often general therapy is combined with novocaine blockade. With careful treatment, pain symptoms can be eliminated for up to a year or even more than a year. In the future, it is advisable to repeat the course of treatment.
Language changes
Language changes can occur as a result of diseases of the gastrointestinal tract, infectious and some other general diseases.
Depending on the type of lesion of the gastrointestinal tract, changes in the tongue may acquire a different character. So, with gastritis, in some cases there is a gray-dirty coating with swelling of the tongue. In most cases, taste sensitivity is reduced. Such changes are especially pronounced during acute gastritis. With a stomach ulcer, the mucous membrane of the tongue is bright red, and with stomach cancer, the tongue becomes pale and atrophic.
One of the most common diseases is desquamative glossitis(geographic language). According to most authors, various diseases of the gastrointestinal tract, exudative diathesis, and helminthic intoxication play an important role in the etiology of this glossitis. Clinical picture this disease is typical. Initially, a whitish-gray spot appears. Gradually, this area, consisting of macerated epithelium, is rejected and islands of bright red color with a smooth, shiny surface are formed. These islets vary in size. They are surrounded by a gray rim, they can merge with each other. In these cases, their boundaries change. The sinuous white-gray outlines resemble a geographical map, hence the second name of this disease. Desquamation of the epithelium is replaced by a fairly rapid epithelialization of individual areas.
Along the edge of the foci, unsharply expressed phenomena of inflammation can be noted. In some cases, patients report dry mouth and burning sensation.
The disease can quickly and without a trace pass. Sometimes it drags on for years.
Treatment. A thorough examination and treatment of the underlying disease is necessary. Baths are used from a 0.5-1% solution of chloramine, novocaine, trimecaine - to relieve pain, ultraviolet irradiation, applications with vitamin A, sea buckthorn oil, 1% solution of citral in peach oil - to accelerate regeneration, multivitamins.
In some cases, language changes are not associated with general diseases of the body. Geographic tongue may be a congenital anomaly of the surface of the tongue.
Folded tongue. In some cases, desquamative glossitis is accompanied. In this case, the tongue is usually enlarged in size due to the thickening of the muscle layer. The folds are located in certain directions. A large furrow runs along middle line along the tongue. It is usually the deepest. Transverse furrows of various lengths depart from it. Folds are observed both superficial and deep. The tongue, in the presence of deep furrows, is divided into separate lobes of various sizes (Fig. 59).
The folded tongue is more often than usual exposed to various injuries - carious teeth, dentures, etc. Food residues, microbes, etc. can accumulate in the folds, which causes discomfort and inflammation. In such cases, a thorough toilet is necessary - washing the folds of the tongue with solutions of potassium permanganate, chloramine, soda.
No special treatment is required.
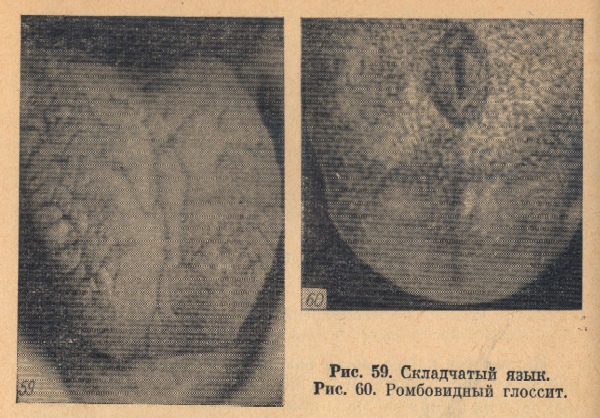
Rhomboid glossitis. This is a chronic disease associated with atrophy and desquamation of the filiform papillae of the tongue.
Changes are usually localized in the region of the posterior third of the back of the tongue. The affected area is diamond-shaped, sharply demarcated from the surrounding mucosa. The surface of the focus is smooth, the papillae of the tongue in this area are atrophied, the tongue is pink or red. In some cases, the lesion rises above the rest of the mucous membrane (Fig. 60) and is covered with a grayish-white coating.
On palpation, there is no difference with the rest of the mucous membrane of the tongue. This change in language is not subject to treatment, although some authors recommend diathermocoagulation.
Lives in the human mouth great amount microorganisms. With regular hygienic care and strong immunity, they do not cause harm, but under the influence of adverse factors, bacteria begin to multiply intensively and cause diseases of the oral cavity.
The entrance to the oral cavity is the lips, on both sides of the face are the mucous membranes of the cheeks. One of important organs in the mouth - the tongue, which is involved in taste perception, salivation, the formation of speech sounds. The gum covers the alveolar process, hard and soft sky take part in diction. The ducts of the salivary glands enter the oral cavity, through which the secret-saliva is secreted. It is essential for the digestion of food.
What are the diseases of the oral cavity in an adult, how to treat them?
Stomatitis
One of the most common ailments is stomatitis. This is an inflammatory disease that affects the mucous membranes of the oral cavity. It is manifested by the formation of vesicles, sores, covered with a whitish, gray or yellow coating.
Most often, oral disease in children and adults - stomatitis manifests itself as a separate disease, but can act as a symptom of concomitant pathology with scleroderma, pemphigus, streptoderma, treatment in such cases is difficult.
The infection is transmitted by airborne droplets or by contact from a sick person to a healthy one. Distinguish acute and. With an exacerbation, the patient's temperature rises sharply, regional lymph nodes increase, ulcers are painful. The chronic form proceeds with less pronounced symptoms, can recur and periodically worsen.
According to clinical manifestations, stomatitis is divided into catarrhal, aphthous, ulcerative, traumatic, angular, allergic, candidal, herpetic, gangrenous.  Stomatitis differs in characteristic rashes, ulcers or aphthae, the presence of necrotic areas of the mucous membrane. called out different types disease different reasons: herpetic stomatitis provokes the herpes virus, candidiasis - yeast fungi of the genus Candida, allergic - an allergy to certain foods or medicines.
Stomatitis differs in characteristic rashes, ulcers or aphthae, the presence of necrotic areas of the mucous membrane. called out different types disease different reasons: herpetic stomatitis provokes the herpes virus, candidiasis - yeast fungi of the genus Candida, allergic - an allergy to certain foods or medicines.
Treatment of stomatitis depends on its form. First of all, eliminate the factors that caused the disease. The oral cavity must be treated with antiseptic solutions, do not eat foods that cause irritation of the mucous membrane. To relieve pain, the affected areas are treated with painkillers. In the presence of an inflammatory process, antibiotic treatment is carried out. With a fungal nature of the disease, antimicrobial drugs are prescribed, with a viral one, antiviral drugs. You can also additionally perform treatment with decoctions of medicinal herbs.
Glossitis
 This is an inflammation of the mucous membrane of the tongue, characterized by a change in its color and structure. Diseases of the tongue in the oral cavity in adults develop when the body is damaged by viruses or microflora is disturbed. Most often develops along with stomatitis.
This is an inflammation of the mucous membrane of the tongue, characterized by a change in its color and structure. Diseases of the tongue in the oral cavity in adults develop when the body is damaged by viruses or microflora is disturbed. Most often develops along with stomatitis.
Symptoms of glossitis:
- Pain, burning in the tongue when talking, while eating.
- Loss of taste sensations.
- Swelling, redness of the tongue.
- Violation of diction.
- The appearance of papillomas, papillary growths on the tongue.
Causes of the disease: tongue injuries, herpes virus, smoking, chronic diseases, poisoning, reduced immunity.
Types of glossitis: deep, desquamative, rhomboid, villous, folded, interstitial, hunter's. They differ in the nature of the plaque, the place of localization in the tongue, and the methods of therapy.
With concomitant chronic diseases, anti-inflammatory treatment is carried out. Soft food that does not irritate the mucous membranes is introduced into the diet. Perform antiseptic mouth rinses severe pain make applications with anesthetics. Plaque from the tongue is removed with a swab soaked in proteolytic enzymes.
Gingivitis

The reason for the formation of the disease is weak immunity, the presence of chronic diseases, injuries of the oral cavity, hormonal imbalance, tartar, poor hygiene, malocclusion.
Distinguish the following forms diseases: catarrhal, atrophic, ulcerative, Vincent's gingivostomatitis, hypertrophic.
Treatment begins with dental cleaning of tartar. If the stage is not running, these measures are enough. Recovery normal microflora perform antibacterial treatment of the mouth. With the development of inflammation, antibiotics are prescribed. Anesthetics are taken to relieve pain. With deep ulcerative, necrotic lesions, surgical treatment is performed.
periodontitis
Oral diseases that affect the periodontal tissues (tissues surrounding the teeth) are called periodontitis. At the same time, not only the gums are involved in the inflammatory process, but also the periodontal ligaments, interalveolar septa. This can lead to the loss of healthy teeth.
 Symptoms of periodontitis:
Symptoms of periodontitis:
- Swelling, redness, soreness of the gums.
- Hypersensitivity, bleeding gums.
- The presence of gum pockets, purulent discharge from them.
- Tooth mobility.
Dental deposits, poor hygiene, hormonal disorders, systemic chronic diseases, beriberi, malocclusion provoke the development of periodontitis.
There are 3 degrees of severity of the disease: mild, moderate, severe. At the initial stage, there is a decrease in the mucous membrane of the gums, exposure of the roots. Later, tooth mobility develops. In severe form, the alveolar process decreases by half, strongly 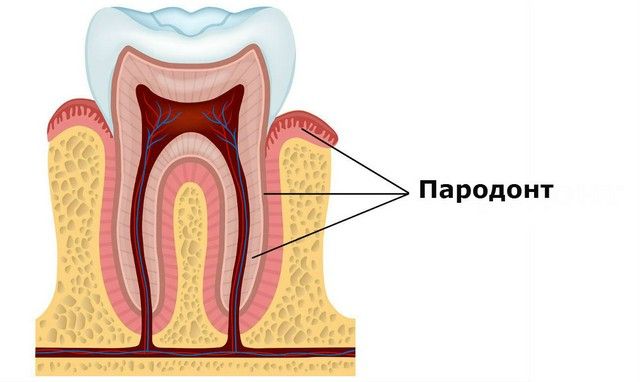 exposing roots. The teeth are highly mobile.
exposing roots. The teeth are highly mobile.
Types of periodontitis: focal, generalized, purulent, aggressive. They differ in the area of tissue damage, the presence of purulent secretions. Advanced stages of the disease can adversely affect the functioning of internal organs.
Diseases of the oral cavity begin to be treated with the removal of tartar. Appointed drug treatment antibiotics, treatment of mucous membranes with painkillers, antiseptic drugs. With the mobility of the teeth, splinting is carried out using a special tape. If the roots are strongly exposed, operations are performed to restore the gingival contour.





