AT oral cavity man lives great amount microorganisms. With regular hygienic care and strong immunity, they do not cause harm, but under the influence of adverse factors, bacteria begin to multiply intensively and cause diseases of the oral cavity.
The entrance to the oral cavity is the lips, on both sides of the face are the mucous membranes of the cheeks. One of important organs in the mouth - the tongue, which is involved in taste perception, salivation, the formation of speech sounds. The gum covers the alveolar process, the hard and soft palate take part in diction. The ducts of the salivary glands enter the oral cavity, through which the secret-saliva is secreted. It is essential for the digestion of food.
What are the diseases of the oral cavity in an adult, how to treat them?
Stomatitis
One of the most common ailments is stomatitis. This is an inflammatory disease that affects the mucous membranes of the oral cavity. It is manifested by the formation of vesicles, sores, covered with a whitish, gray or yellow coating.
Most often, oral disease in children and adults - stomatitis manifests itself as a separate disease, but can act as a symptom of concomitant pathology with scleroderma, pemphigus, streptoderma, treatment in such cases is difficult.
The infection is transmitted by airborne droplets or by contact from a sick person to a healthy one. Distinguish acute and. With an exacerbation, the patient's temperature rises sharply, regional lymph nodes increase, ulcers are painful. The chronic form proceeds with less pronounced symptoms, can recur and periodically worsen.
According to clinical manifestations, stomatitis is divided into catarrhal, aphthous, ulcerative, traumatic, angular, allergic, candidal, herpetic, gangrenous. 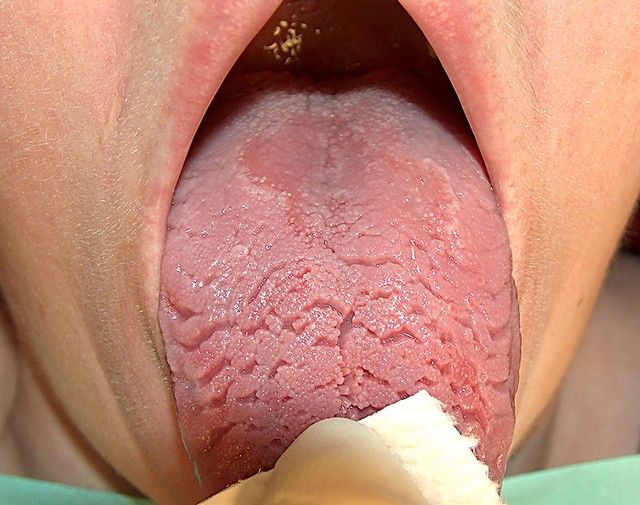 Stomatitis differs in characteristic rashes, ulcers or aphthae, the presence of necrotic areas of the mucous membrane. called out different types diseases for various reasons: herpetic stomatitis provokes the herpes virus, candidiasis - yeast fungi of the genus Candida, allergic - an allergy to certain foods or medicines.
Stomatitis differs in characteristic rashes, ulcers or aphthae, the presence of necrotic areas of the mucous membrane. called out different types diseases for various reasons: herpetic stomatitis provokes the herpes virus, candidiasis - yeast fungi of the genus Candida, allergic - an allergy to certain foods or medicines.
Treatment of stomatitis depends on its form. First of all, eliminate the factors that caused the disease. The oral cavity must be treated with antiseptic solutions, do not eat foods that cause irritation of the mucous membrane. To relieve pain, the affected areas are treated with painkillers. In the presence of an inflammatory process, antibiotic treatment is carried out. With a fungal nature of the disease, antimicrobial drugs are prescribed, with a viral one, antiviral drugs. You can also additionally perform treatment with decoctions of medicinal herbs.
Glossitis
 This is an inflammation of the mucous membrane of the tongue, characterized by a change in its color and structure. Diseases of the tongue in the oral cavity in adults develop when the body is damaged by viruses or microflora is disturbed. Most often develops along with stomatitis.
This is an inflammation of the mucous membrane of the tongue, characterized by a change in its color and structure. Diseases of the tongue in the oral cavity in adults develop when the body is damaged by viruses or microflora is disturbed. Most often develops along with stomatitis.
Symptoms of glossitis:
- Pain, burning in the tongue when talking, while eating.
- Loss of taste sensations.
- Swelling, redness of the tongue.
- Violation of diction.
- The appearance of papillomas, papillary growths on the tongue.
Causes of the disease: tongue injuries, herpes virus, smoking, chronic diseases, poisoning, reduced immunity.
Types of glossitis: deep, desquamative, rhomboid, villous, folded, interstitial, hunter's. They differ in the nature of the plaque, the place of localization in the tongue, and the methods of therapy.
With concomitant chronic diseases, anti-inflammatory treatment is carried out. Soft food that does not irritate the mucous membranes is introduced into the diet. Perform antiseptic mouth rinses, with severe pain, make applications with anesthetics. Plaque from the tongue is removed with a swab soaked in proteolytic enzymes.
Gingivitis

The reason for the formation of the disease is weak immunity, the presence of chronic diseases, injuries of the oral cavity, hormonal imbalance, tartar, poor hygiene, malocclusion.
Distinguish the following forms diseases: catarrhal, atrophic, ulcerative, Vincent's gingivostomatitis, hypertrophic.
Treatment begins with dental cleaning of tartar. If the stage is not running, these measures are enough. Recovery normal microflora perform antibacterial treatment of the mouth. With the development of inflammation, antibiotics are prescribed. Anesthetics are taken to relieve pain. With deep ulcerative, necrotic lesions, surgical treatment is performed.
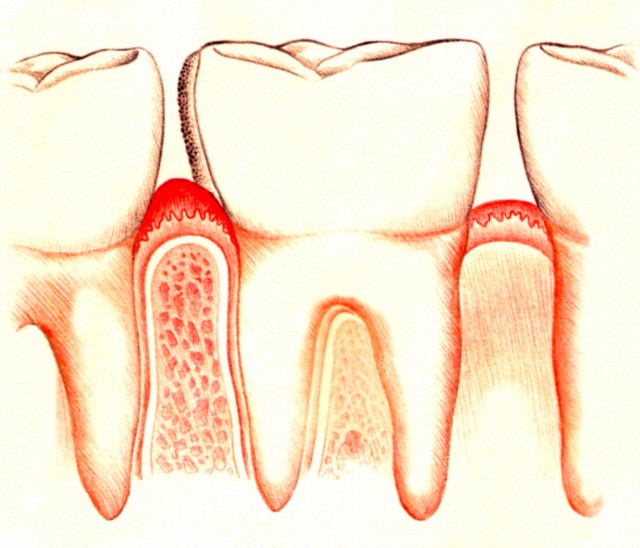
periodontitis
Oral diseases that affect the periodontal tissues (tissues surrounding the teeth) are called periodontitis. At the same time, in inflammatory process not only the gums are involved, but also the periodontal ligaments, interalveolar septa. This can lead to the loss of healthy teeth.
 Symptoms of periodontitis:
Symptoms of periodontitis:
- Swelling, redness, soreness of the gums.
- Hypersensitivity, bleeding gums.
- The presence of gum pockets, purulent discharge from them.
- Tooth mobility.
Dental deposits, poor hygiene, hormonal disorders, systemic chronic diseases, beriberi, malocclusion provoke the development of periodontitis.
There are 3 degrees of severity of the disease: mild, moderate, severe. At the initial stage, there is a decrease in the mucous membrane of the gums, exposure of the roots. Later, tooth mobility develops. In severe form, the alveolar process decreases by half, strongly 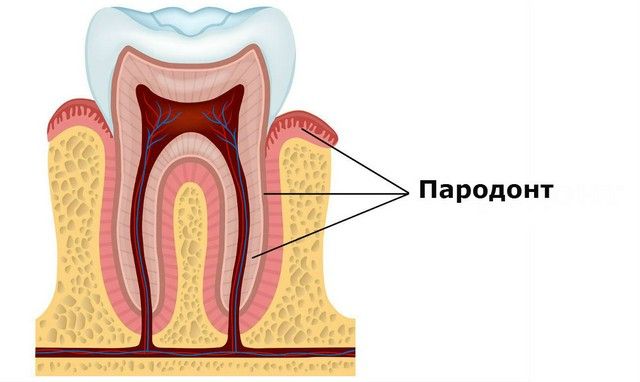 exposing roots. The teeth are highly mobile.
exposing roots. The teeth are highly mobile.
Types of periodontitis: focal, generalized, purulent, aggressive. They differ in the area of tissue damage, the presence of purulent secretions. Advanced stages of the disease can adversely affect work internal organs.
Diseases of the oral cavity begin to be treated with the removal of tartar. Appointed drug treatment antibiotics, treatment of mucous membranes with painkillers, antiseptic drugs. With the mobility of the teeth, splinting is carried out using a special tape. If the roots are strongly exposed, operations are performed to restore the gingival contour.
The mucous membrane lining the oral cavity consists of stratified squamous epithelium with a basement membrane, its own and submucosal layers. The ratio of these layers in different parts of the oral cavity is not the same. In some areas there is a more powerful epithelial layer (hard palate, tongue, gums). In others, the proper mucous membrane (lips, cheeks) is well expressed. In the third areas, the submucosal layer is more developed (bottom of the oral cavity, transitional folds). Throughout the oral mucosa is covered with stratified squamous epithelium.
The epithelial layer is directly facing the oral cavity and, due to the desquamation of the upper layers of cells, is subject to constant renewal.
Classification of diseases of the mucous membrane
1. traumatic lesions (mechanical, chemical, physical) - traumatic erythema, erosion, ulcer, lecoplakia, non-catinic lecokeratosis, actinic cheilitis, radiation and chemical injuries.
1) Viral (herpetic stomatitis, shingles, foot and mouth disease, viral warts, influenza, HIV infection)
2) Ulcerative necrotic stomatitis of Vincent.
3) Bacterial infections (streptococcal stomatitis, pyogenic granuloma, chancriform pyoderma, tuberculosis, etc.).
4) Sexually transmitted diseases (syphilis, gonorrheal stomatitis).
5) Mycoses (candidiasis, actinomycosis)
3. Allergic diseases (Quincke's edema, allergic stomatitis, cheilitis, glossitis, drug-induced cheilitis, stomatitis, glossitis, erythema multiforme exudative, recurrent aphthous stomatitis, etc.).
4. Changes in the oral mucosa during exogenous intoxications
5. Changes in the oral mucosa in some systemic diseases and metabolic diseases (hypo and beriberi, endocrine diseases, diseases of the gastrointestinal -intestinal tract, cardiovascular system, blood system, nervous system, rheumatic diseases, collagenoses.)
6. Mucosal changes in dermatoses (pemphigus, lichen planus, lupus erythematosus)
7. Anomalies and independent diseases of the tongue (folded tongue, black "hairy" tongue, rhomboid and desquamative glossitis)
8. Independent cheilitis (glandular, exfoliative, actinic, meteorological, atopic, eczematous, contact, macrocheilitis).
9. Precancerous diseases (obligate and facultative) and tumors (benign and malignant).
Elements of mucosal damage
There are primary and secondary (developing from primary) elements.
The primary ones include a spot, a nodule, a node, a tubercle, a vesicle, a bubble, an abscess, a cyst, a blister, an abscess.
A stain is a formation resulting from the deposition of pigment or coloring matter. Spots are of inflammatory origin - roseola, hemorrhages, erythema.
A nodule is a cavityless formation protruding above the surface of the skin.
The node is a dense formation, a small infiltrate of a rounded shape.
A tubercle is an infiltrative, cavityless formation that captures all layers of the mucosa.
A bubble is a cavity element resulting from a limited accumulation of fluid.
Bubble - unlike the bubble, larger.
An abscess is a cavity formation made by a purulent
exudate.
Secondary elements - erosion, aphtha, ulcer, crack, scar, plaque, scales, crust atrophy.
Erosion is a violation of the integrity of the epithelium, resulting from the destruction or opening of the primary cavity formations. Heals without scarring.
Aphtha is a superficial defect of the epithelium, located on the inflamed area of the mucosa.
Ulcer - characterized by a violation of all layers of the mucosa, heals with the formation of a scar.
A fissure is a linear defect within the epithelium only.
Scales - falling off plates of keratinized epithelial cells, formed as a result of pathological keratinization.
Crust - dried exudate of vesicles, pustules, cracks, ulcers.
A tumor is an overgrowth of tissue due to excess cell reproduction.
Traumatic papillomatosis is the growth of the papillary layer of the mucosa, protruding above its level. A long-term injury can lead to keratinization of individual sections of the mucosa.
In some cases, bleeding and inflammation occur. When exposed to mechanical trauma, edema and hyperemia primarily occur. Then erosion or a decubital ulcer may appear at this site. As a rule, this is a single painful ulcer, surrounded by an inflammatory infiltrate, covered with a fibrinous coating. With a long course of it, malignancy is possible.
Leukoplakia - keratinization of the oral mucosa with its chronic irritation. The disease is accompanied by a thickening of the epithelial layer, with a change in color and involvement of the mucous layer itself in the inflammatory process.
1. leukoplakia of smokers - keratinized areas of the hard and soft palate, clouding of the mucosa throughout the keratosis area and the transition to normal mucosa without clear boundaries. Elements do not protrude above the level of the mucosa.
2. simple leukoplakia - keratinization foci of various shapes and with a clear boundary. More often localized on the buccal mucosa.
3. verrucous - there is a more significant keratinization, the elements of the lesion rise above the mucosa, they are painful especially during meals.
4. erosive-ulcerative - in addition to the foci characteristic of the simple and vercous forms of leukoplakia, erosions and ulcers appear. Pain symptoms are more pronounced.
5. soft - edematous areas of peeling with soft hyperplastic plaque, complaints about the roughness of the mucous membrane and its peeling, change in taste.
Treatment. Elimination of annoying factors. Mandatory appointment of multivitamins, sanitation of the oral cavity. Inside prescribe vit.A, E, as well as applications with oil solutions of these vitamins. Sometimes it is necessary to resort to surgical excision of foci of leukoplakia. Subsequently, keratoplasty is prescribed.
Acute herpetic aphthous stomatitis is a manifestation of primary infection with the herpes simplex virus. The elements that appear on the mucous membrane resemble aphthae that occur against the background of catarrhal inflammation. The disease is contagious, proceeds as an acute infectious process with high temperature and general disorder. In the pathogenesis, periods are observed: prodromal, catarrhal, rashes and extinction of the disease. According to severity, mild, moderate and severe forms are distinguished.
Usually the course of the disease is characterized by severe symptoms of toxicosis. In the prodromal period, malaise, weakness, headache, nausea are observed. Body temperature reaches 38-38.5 °C. submandibular lymph nodes are enlarged, painful. The mucous membrane is edematous and hyperemic, saliva is viscous and viscous. On the 4-5th day, multiple aphthous rashes appear.
Acute herpetic stomatitis, like a number of others viral diseases may heal spontaneously. Tactics of treatment is determined by the severity and period of development of the disease. Treatment includes the use of antiviral (bonafton, acyclovir, DNase, leukocyte interferon, etc.), desensitizing (suprastin, fenkarol, tavigil, etc.) and anti-inflammatory (florenal, tebrofen, antiseptic solutions, etc.) drugs from the first days of the disease and symptomatic therapy. Proteolytic enzymes, vitamins, keratoplasty are also prescribed.
STOMATITIS, CHEILITS. CLINIC. TREATMENT. PREVENTION
1. Erosive stomatitis
2. Ulcerative-necrotic stomatitis of Vincent
3. Gangrenous stomatitis
4. Gonorrheal stomatitis
5. Chronic recurrent aphthous stomatitis
6. Exfoliative cheilitis
7. Actinic cheilitis
8. Meteorological cheilitis
9. Chronic cracked lip
10. Glandular cheilitis
11. Lymphedematous macrocheilitis
12. Contact allergic cheilitis
13. Eczematous cheilitis
14. Atopic cheilitis
15. Misher's granulomatous cheilitis
16. Lichen planus
17. Hypovitaminosis C
18. Hypovitaminosis A
19. Hypovitaminosis RR
20. Hypovitaminosis B 1
21. Hypovitaminosis B 2
1. Erosive stomatitis- an infectious disease, the causative agent of which is diplococcus. The disease develops after suffering the flu, tonsillitis or other infection. Incubation period 2-6 days.
Clinic. Patients complain of itching, burning, soreness in the oral cavity during meals. The elements of the lesion are erosion and erythema, round, 2-3 mm in diameter, which merge into larger ones (up to 20 mm). There are no deposits and films on the erosion surface. The skin is never involved in the process. The duration of the disease is 4-10 days. The prognosis is favorable.
Treatment. Locally - antiseptics and local anesthetics, anti-inflammatory and keratoplastic drugs. General - antibiotics, sulfonamides.
2. Ulcerative necrotic stomatitis of Vincent- an infectious inflammatory disease that occurs against the background of a reduced reactivity of the body in the presence of adverse conditions in the oral cavity and is characterized by necrosis and ulceration.
Called by Vincent's spirochete and fusiform bacillus, it is a saprophyte of the oral cavity. It develops against the background of hypothermia, stress, injuries (sharp edges of decayed teeth, deep-set artificial crowns, difficult eruption of wisdom teeth). It can be a symptom of diseases of the blood, gastrointestinal tract, and other organs and systems.
Allocate acute, subacute, chronic and mild, moderate and severe forms.
Clinic. Bleeding gums, burning and dryness of CO, hypersalivation, weakness, headache, subfibril temperature, joint pain. Ulceration begins in areas where there are irritating factors. Further on the adjacent areas up to necrosis. There is a putrid odor from the mouth. SO is edematous, loose, hyperemic, sharply painful, bleeding.
Treatment. Local: in the hydration phase - anesthesia, antiseptic treatment, surgical treatment, necrolytic agents, anti-inflammatory agents; in the phase of dehydration - stimulants of reparative processes, sanitation of the oral cavity. General: antibiotics, anti-inflammatory, hyposensitizing, vitamins, detoxification agents.
3. Gangrenous stomatitis- necrotic damage to the CO, which develops as a result of vascular and trophic disorders caused by anaerobic infection.
Clinic. Severe general condition, intoxication, deep necrosis with decay of all CO layers and rapid spread of the process.
Treatment. General - detoxification and antibacterial therapy. Local - according to the principles ulcerative necrotic stomatitis.
4. Gonorrheal stomatitis- an acute infectious disease, the causative agent of which is gonococcus. Incubation period - 1 - 30 days. Inflammation with the formation of purulent exudate and gray plaque.
Treatment. Antimicrobial therapy and the same as with purulent-necrotic lesions of CO.
5. Chronic recurrent aphthous stomatitis- an allergic disease, manifested by a rash of single aphthae, which recur without definite patterns and are characterized by a long course.
Factors causing the disease: adenovirus, staphylococcus aureus, allergies, immune disorders, diseases of the organs and systems of the gastrointestinal tract, neurotrophic disorders, genetic conditioning, the influence of harmful factors.
Clinic. Complaints about the rash of painful aphthae. Unsystematic relapses. On examination, aphthae are round or oval in shape with a narrow rim of inflammatory hyperemia of a bright red color, covered with a gray-white fibrous coating and sharply painful. Allocate light, medium and heavy forms. Cycle - 7 - 10 days.
Treatment. Local: sanitation of the oral cavity, treatment of aft with anesthetics, necrolytic, antiseptic, anti-inflammatory, keratoplastic agents. General: hyposensitizing, detoxification therapy, vitamin therapy, drugs that improve nervous trophism.
cheilite- inflammation of the red border, mucous membrane and skin of the lips.
b. Exfoliative cheilitis- a chronic disease of the exclusively red border of the lips, which is accompanied by peeling of epithelial cells due to a violation of their keratinization, against the background of a dysfunction of the nervous system.
There are dry (flat thin scales on the border of the red border and CO) and exudative forms (massive gray-yellow or yellow-brown crusts form on the hyperemic, edematous red border). The disease proceeds for a long time (years, sometimes tens of years), is not prone to self-healing.
Treatment. Exudative - boundary rays of Bucca and drugs that increase the reactivity of the body. Dry - indifferent ointments and creams, hygienic lipstick.
7. Actinic cheilitis- chronic inflammation of the lips with increased
sensitivity of the red border to sunlight.
The reason is ultraviolet rays in the presence of sensitization to sunlight.
Clinic. There are dry (the red border is dry, bright red, covered with silver-white scales) and exudative forms (bubbles appear against the background of the edematous bright red border, which quickly open, forming erosion, crusts and cracks).
Treatment. Avoid sun exposure. Locally - corticosteroid ointments, photoprotective creams. Inside - group vitamins AT.
8. Meteorological cheilitis- inflammatory disease of the lips, caused by the action of meteorological factors (high or low humidity, wind, cold, dusty air, sunlight and etc.).
Clinic. It is more common in men, in people with delicate skin and in diseases accompanied by increased dryness of the skin. The red border of the lips is stagnantly hyperemic, infiltrated, dry, covered with small scales. It proceeds chronically and does not depend on the time of year.
Treatment. Eliminate the irritating effect of meteorological factors. Assign nicotinic acid, vitamins of group B. Locally - lubrication of the lips with protective ointments, hygienic lipstick.
9. Chronic cracked lip- limited inflammation with a defect in the slit-like form of the epithelium and the lamina propria.
The reason is a feature of the individual structure and chronic trauma, meteorological factors, hypovitaminosis. The microbial flora supports the existence of cracks and prevents their healing.
Clinic. Single different depth, linear crack. Never transfers to the skin. The fissure is covered with a bloody crust, surrounded by a hyperemic border. May recur, margins may become keratinized.
Treatment. Eliminate the cause of the disease. Locally - ointments with antibiotics, corticosteroids, agents that stimulate epithelialization. General - vitamins of groups A and B. In the absence of effect, surgical excision of a crack within healthy tissues.
10. Glandular cheilitis- a disease caused by inflammation of the small salivary glands moved to the red border, their hypertrophy and hyperfunction.
Inflammation can be serous (swelling of the lips, congestive hyperemia, tuberosity, dryness, peeling, cracks, erosion) or purulent (develops due to infection entering the ducts). It is characterized by soreness, swelling, enlargement of the lip, which is covered with tightly fixed crusts of yellow-green or brown-black color, cracks and erosion form around the excretory ducts.
Treatment. Surgical - removal of the entire area with displaced glands. Deep coagulation of the bodies of the salivary glands. Before surgical treatment, cracks, erosions, and crusts are eliminated.
11. Lymphedematous macrocheilitis- a disease associated with impaired lymph circulation caused by sensitization of the body by microflora from foci of chronic infection.
Clinically manifested by painless lip enlargement. The course is chronic with exacerbations. There are early, advanced and late stages.
Treatment. In the early stages - thermal procedures, paraffin therapy, special massages, sclerotherapy, inside - potassium iodide. In the advanced stage - surgical treatment.
12. Contact allergic cheilitis- lip disease that develops
due to tissue sensitization to various chemicals.
Reason - chemical substances, which are part of lipsticks, toothpastes, plastics of dentures, etc.
The clinic is hyperemia and swelling of the red border of the lips with finely scaly peeling, cracks, vesicles and erosions.
Treatment. Elimination of the chemical factor, corticosteroid ointments, desensitizing therapy.
13. Eczematous cheilitis - a chronic allergic disease of the red border and skin of the lips.
It occurs as an isolated lesion and as a symptom of facial eczema. Allergens can be microorganisms, food substances, medicines, metals, denture materials, toothpaste components, etc.
Clinic. The disease has an acute (polymorphism of the elements of the lesion - redness, small vesicles that merge to form ring-shaped scales and crusts, itching, swelling) and a chronic course (chronic swelling, hyperemia, dry peeling, cracks, bloody crusts. The process lasts for years with exacerbations.
Treatment. Desensitizing, vitamin therapy. Locally - corticosteroid ointments.
14. Atopic cheilitis- a symptom of dermatitis or neurodermatitis.
It occurs in children and adolescents aged 7-17 years with a tendency to atopic allergies.
Clinic. The red border and the skin of the lips are affected more often in the corners of the mouth. Manifested by itching, erythema, edema, inflammation of adjacent areas, infiltration, dryness, cracking. After the subsidence of acute phenomena, peeling appears.
Treatment. Desensitizing therapy, vitamins, sedatives, oral and topical corticosteroids.
15. Misher's granulomatous cheilitis- persistent inflammatory thickening
lips.
The reason is not clear. The course is chronic with exacerbations. Treatment. Surgical removal of diseased tissue.
16. Lichen planus- chronic disease of the skin and mucous membranes
membranes with the formation of keratinized papules.
Causes: heredity, infection, drugs, physical and chemical factors, diseases of the nervous system, endocrine and metabolic disorders, immunological mechanisms.
The course is chronic with exacerbations. Distinguish hyperkeratotic (typical) shape: whitish papules with a keratinized top, which merge into a grid;
erosive form: pain and burning, bleeding, focus of papules with erythema and erosion; ulcerative form: pain, difficulty opening the mouth, bad breath, among the accumulation of papules there is a shallow ulcer with jagged edges;
pemphigoid form: anamnesis burdened with hypertension, chronic nephropathies, rheumatic heart disease, chronic tonsillitis, there are papules in the oral cavity white color with a pearly tint, which merge into a grid with blisters and erosions, a banal or fungal infection may join;
warty shape: papules form painless warty growths with a reticulate pattern of keratinized papules.
Treatment is aimed at eliminating keratosis, inflammation and normalizing the process of keratinization of the epithelium and eliminating complications (erythema, erosion, ulcers, blisters, warts). General - sedatives, desensitizing agents, vitamin therapy, physiotherapy, a diet that excludes smoking, alcohol, spicy and hot food. Locally - sanitation of the oral cavity (elimination of dental deposits, galvanosis, sharp edges of teeth, correction of dentures, treatment of periodontal diseases), use materials with a high degree indifference and correctly model the occlusal surface to prevent injury along the line of teeth closure. Treatment of the focus - rinses, vitamins, cryodestruction, surgical treatment, keratinizing ointments, solutions, corticosteroid therapy.
CO changes in hypo- and avitaminosis- develops with insufficient intake of vitamins from food or a violation of their absorption. Isolated forms of insufficiency of one of the vitamins are rare, more often - insufficiency of several vitamins.
17. Hypovitaminosis C- leads to a violation of metabolic processes, a decrease in the reactivity of the body, growth processes, a sharp violation of the processes of capillary permeability.
There are three stages: scurvy stomatopathy - initial - pronounced gingivitis against the background of pale anemic CO, bleeding; scurvy reparative stomatitis - an advanced stage - is characterized by significant inflammation of the gums, swelling, loosening, cyanotic color, bleeding, tooth mobility; scurvy ulcerative stomatitis - a complicated stage - occurs due to the addition of a secondary infection, accompanied by the growth of granulations reaching the cutting edge or chewing surface of the teeth, with areas of necrosis and ulceration, bleeding, necrotic plaque with a fetid odor and the spread of the process to the tongue, cheeks, lips, hard and soft palate, loosening and loss of teeth. The general condition is extremely serious and without treatment can be fatal.
Treatment. General - prescribe vitamin C in various types and vitamin R. Local - sanitation of the oral cavity, hygiene, irrigation of the oral cavity with vitamin solutions. At the height of the disease, the removal of granulations and teeth is contraindicated.
18. Hypovitaminosis A- the processes of growth and development of the organism, the maturation of the epithelium and its keratinization worsen, the resistance of CO to traumatic and irritating factors decreases.
Clinic. SA is pale, cloudy, dry. On the cheeks, hard and soft palate whitish layers, dry throat, bluish lips, with increased epidermization. Treatment. Vitamin A and foods rich in vitamin A are prescribed.
19. Hypovitaminosis RR- redox processes, metabolism of carbohydrates and proteins worsen. pellagra develops. In the oral cavity: stage 1 - the occurrence of erythema - burning in the lips, cheeks, tongue, CO is hyperemic, swollen tongue, atrophied filiform papillae, weakness, headache, insomnia, loss of appetite; stage 2 - pain in the oral cavity of the neuralgic type, the process extends to the entire oral cavity, the tongue is bright red, swollen, crimson, shiny, smooth, mirror-like with cracks, the general condition worsens; Stage 3 - the general condition is severe, a secondary infection joins and ulcerative stomatitis develops.
Treatment. Saturation of the body with nicotinic acid and vitamins of group B. Local - thorough sanitation of the oral cavity, hygienic rinses, elimination of irritants, local anesthetics, antiseptics, prosthetolysis enzymes, keratoplastic preparations.
20. Hypovitaminosis B1 beriberi disease, which develops in individuals
consuming predominantly carbohydrate food and with insufficient absorption in
intestines.
Clinic. The defeat of the nervous and cardiovascular systems, the development of edema. It may be accompanied by trigeminal neuralgia, increased pain sensitivity of CO, pain in the teeth, jaws, ulcers, bubble lesions of CO are encountered.
Treatment. Saturation of the body with thiamine and proteins. Local - symptomatic.
21. Hypovitaminosis B2 - a disease with inflammation of the lips (angular cheilitis), glossitis, conjunctivitis.
Clinic. It starts with redness in the corners of the mouth, then painful cracks appear, like jams. The lips become red, swollen, cracks and erosion appear. At the same time, glossitis develops with severe pain, atrophy of the filiform papillae, and hypertrophy of the mushroom papillae.
Treatment. Saturation of the body with vitamins of group B. Local - symptomatic.
HIV infection in the oral cavity.
After being infected with HIV within 5 years, AIDS develops in 20% of infected individuals, and in 50% within 10 years. However, the acute phase of HIV can appear as early as a few weeks. Oral mucosal diseases associated with HIV infection include:
1. different clinical forms of candidiasis
2. viral infections
3. hairy leukoplakia
4. ulcerative necrotic gingivostomatitis
5. progressive form of periodontitis
6. Kaposi's sarcoma
The most common symptom of HIV infection is candidiasis. On the mucous membrane there is a grayish-white cheesy coating. Possible candidal angular cheilitis and fissures.
Hairy leukoplakia was observed in 98% of HIV patients. Clinically, it looks like folds and villi of white color, rising above the surface of the mucosa, in shape they resemble hair. These villi cannot be scraped off. Most often, this leukoplakia is localized on the lateral surfaces of the tongue.
Kaposi's sarcoma is the most characteristic symptom of the disease. The tumor is formed from the lymphatic vessels. In the oral cavity, it is most often localized in the sky, less often on the gum mucosa. It has the appearance of bluish, reddish or black spots, which further grow and ulcerate. Kaposi's sarcoma closely resembles epulis.
Diseases that should alert the dentist regarding HIV infection of the patient include squamous cell carcinoma of the oral mucosa, lymphoma.
1. stage. Asymptomatic. Or lymphadenopathy (an increase in nodes in diameter in 2 or more areas.
2. stage. AIDS related complex. Characteristic: weight loss, diarrhea, fatigue, drowsiness, loss of appetite. In this stage, there are such manifestations of HIV as hairy leukoplakia, herpes zoster, exacerbation of chronic recurrent herpes.
3. stage. Intermediate stage of the disease. At this stage, candidiasis, hairy leukoplakia, exacerbation of chronic herpes, pulmonary tuberculosis, alveolar pyorrhea appear.
4. stage. late stage. Characterized by diseases caused by protozoal invasions, fungal, viral and bacterial infections, severe forms of lymphoma, cachexia, neurological disorders.
Syphilis is a chronic infectious disease caused by Treponema pallidum. The mucous membrane of the oral cavity is the site of localization of syphilitic eruptions in all periods of syphilis.
During syphilis, 4 stages are distinguished - incubation, primary, secondary and tertiary. incubation period. 21-24 days.
primary period. 6-8 weeks Begins with the appearance of a hard chancre at the site of infection. This is an ulcer that has a round or oval shape with smooth edges, a cartilage-like infiltrate of the chancre is covered with a grayish coating. During this period, pale treponema intensively multiply in the lymph nodes, which is characterized by severe polyadenitis.
The secondary period of syphilis (3-4 years) manifests itself in the oral cavity in the form of roseola and papules. Roseolas often appear on the palatine arches, soft palate or tonsils, as a result of which erythematous tonsillitis occurs, while there are no banal pain sensations.
Papular syphilis is the most common manifestation of secondary syphilis. Papular rashes can be observed over the entire surface of the mucosa. On the mucous membrane of the tongue, they often resemble foci of desquamation. The papules are covered with a gray coating, which, when removed, reveals a bright red, painless surface. Pain can only occur when they are ulcerated.
The tertiary period (4-6 years) of syphilis manifests itself in the form of gums and bumpy rashes. Gummas single or multiple can be localized anywhere in the mucosa. Initially, a painless node appears, which then enlarges, ulcerates and opens with the formation of an ulcer, which in turn heals with the formation of a retracted scar. This period is also characterized by the occurrence of syphilitic glossitis. At the same time, the tongue acquires greater density and becomes inactive. The tongue is covered with trophic ulcers, which can become malignant in the future.
Tuberculous syphilis is most often localized on the lips and is a bluish-red tubercles that disintegrate with the formation of ulcers.
Oral diseases are very common. Suffice it to say that they occur in almost all adults and 70 percent of children. Most of them are characterized by pathological processes of an inflammatory nature.
The oral mucosa is reliable protection body and has a close relationship with a number of internal organs and systems. Most diseases can provoke different reasons. This includes various injuries, such as burns from hot food, dehydration, reduced immunity, lack of important vitamins and minerals, allergies, infectious components, tartar, poor oral care.
Of all the numerous diseases that can form in the mouth, infectious-inflammatory, fungal and viral, dental diseases should be distinguished, dividing them into appropriate groups. In addition, there are a number of manifestations that are difficult to attribute to any of the listed groups. They will also be discussed below.
As you know, any disease has its own characteristics. This helps to determine not only the choice of a specialist, but also to find out which pathology can be cured by oneself, and which one can only be cured by a specialist. Below are some of the most known diseases oral cavity.
Viral diseases
Human papillomaviruses and herpes viruses can cause the formation of these pathologies of the patient's oral cavity.
Herpes. It is considered one of the most common diseases. Studies show that about ninety percent of people are infected with this virus. Often it is localized in the body, taking a latent form. If the patient's immune defenses function well, then herpes in most cases manifests itself as a small pimple that resolves without outside interference in short term, which is usually no more than seven to ten days. When the immune system is weakened, the disease takes on more serious forms.
Being at rest, the disease begins to take an active form with such provoking factors:
- stress;
- a cold;
- not observing sleep patterns, lack of sleep,
- climatic: in cold, windy weather;
- menstruation
- surgical interventions,
- immunosuppression.
The process of development of the disease occurs in stages and includes, as a rule, six stages. The first signs that make themselves felt are characterized by itching on the lips and slight tingling in this area. Then the lips become swollen, reddish and painful sensations appear that interfere with eating and talking. The next stage is characterized by the appearance of scattered small bubbles or entire groups of such bubbles. After some time, the bubbles begin to burst, turning into tiny ulcers. They have a hard crust that often cracks. The final stage is the gradual passage of ulcers and the disappearance of redness, as well as pain.
If the first symptoms of herpes are found, it is necessary to apply something cold, preferably an ice floe, to the lips. And also treat with a high-quality balm for moisturizing. Subsequently formed small bubbles need to be lubricated with an ointment intended for this, which is always possible to purchase at any point in the pharmacy network. Good help, for example, penciclovir. With frequent exposure of the patient to exacerbations of this disease (on the recommendation of a doctor), antiviral agents can be taken.
Papilloma. it famous education can, caused by the papillomavirus, form on different areas body. There are several types of viruses, but one of them (human papilloma) can cause the manifestation of the disease in the oral cavity. There, these formations look like white plaques. Papillomas may represent serious danger, especially when spreading to the throat area, when the patient has problems not only with hoarseness, but also with breathing. Besides this species The virus is not completely cured, you can only eliminate the clinical manifestations by one of the methods:
- surgical intervention;
- in a chemical way;
- cytostatic;
- using immunotherapy.
This does not exclude the possibility of combining the above methods.
Infectious and inflammatory diseases
This nature of the disease is a very common reason for patients to turn to various kinds of specialists - therapists, dentists or otolaryngologists. The following conversation will be about the most common diseases of an infectious-inflammatory nature.
Pharyngitis. It is characterized by inflammation of the mucous membrane of the pharynx and, in particular, the throat. Accompanying the disease, as a rule, is perspiration, a feeling of discomfort when eating and acute pain in the throat.
Acute pharyngitis. There are many reasons for its manifestation. The development of the process can be provoked by cold or polluted air that the patient inhales, tobacco smoke, various chemicals. In addition, the presence of pneumococcal infection can also affect the development of pharyngitis. In addition to those named common features pharyngitis, one can also name such as general weakness, an increase in body temperature, while its increase is noted only in acute case. For the chronic form, such a symptom is not typical.
As a rule, the diagnosis of this disease is carried out by the method of a general examination by a specialist and taking a swab from the throat. Specialists prescribe the treatment of pharyngitis with antibiotics only in exceptional cases, when the disease has complex nature currents. Basically, it is sufficient for the patient to follow a certain diet, taking hot foot baths. Warm compresses on the neck, inhalations and warm milk with honey are excellent help to overcome the disease.
Glossitis. This disease is characterized by an inflammatory process, as a result of which the structure and color of the tongue changes. Provoking factors in most cases are infections of the oral cavity. Others can also influence the manifestation of the disease. various reasons, for example, a tongue burn, excessive alcohol addiction, oral injuries, as they are a kind of infection passers. In addition, often among the sick people with this disease are patients who abuse spicy food and low-quality mouth fresheners. Of course, the risk of getting glossitis increases significantly in patients who do not follow the basic rules of hygiene, for example, who use other people's accessories for brushing their teeth.
Among the signs of the disease can be called the presence of a burning sensation, a feeling of discomfort. Then, after some time, the patient's tongue takes on a pronounced red color, the process of salivation is activated. After some time, signs of the disease will be a dullness or complete absence of taste. At the same time, in some cases, taste sensations do not disappear, but become perverted.
In the absence of timely and high-quality treatment, the consequences can be the most severe, because the tongue can swell so much that it will be difficult for the patient not only to eat, but also to talk. In addition, growths can cover the entire tongue. As a rule, the treatment of glossitis is to take medications, as well as to follow a special diet, which is based on liquid food.
Stomatitis. When they talk about infectious diseases oral cavity, the first thing they mean is the most common stomatitis among them. The patient is infected different ways. This can happen, for example, as a result of a mechanical injury. When the infection enters the patient's body, ulcers begin to form, which have signs that are unique to stomatitis. In most cases, they begin to form inside the cheeks and lips, spread to the root of the tongue and under it. The characteristic of ulcers may be in a shallow form. They can be single and round with even edges, covered with a film in the center. In most cases, these formations are very painful.
When treating stomatitis, the patient should use special toothpastes and rinses. They should not contain sodium lauryl sulfate. With severe pain, it is recommended to use anesthetics. In addition, there are special tools that help remove the film from the sores, which significantly reduces the treatment time. This disease also involves the use of drugs for infection, which the doctor will prescribe.
Herpes and stomatitis: what is the difference
Often, even doctors cannot immediately distinguish stomatitis from viral herpes, as a result of infection, painful sores form in the patient's mouth. Currently, the distinction is made according to some significant features characteristic of this particular pathology:
- if stomatitis is constantly localized in new areas, then herpes does not tend to choose other affected areas, appearing in the same place;
- stomatitis in most cases is localized on soft tissues, while herpes, as a rule, affects tissue areas adjacent to bone structures;
- with herpes, the manifestation of ulcers begins after the bursting of small blisters, with stomatitis, the inflammatory process begins with the formation of ulcers.
Gingivitis. This pathology is an inflammation of the mucous membrane of the gums. Occurs quite often. This is a disease that affects women during pregnancy and adolescent patients to a greater extent.
Currently, gingivitis is divided into four types:
- catarrhal. The most characteristic signs are bleeding with swelling and redness of the gums, itching;
- ulcerative necrotic. It is characterized by the appearance of ulcers and necrosis on the gums. Also hallmarks inherent in this type of gingivitis are such as the presence of halitosis, acute pain, swollen lymph nodes. In addition, the patient experiences general malaise, an increase in temperature;
- hypertrophic. With this type of disease, one can observe an increase in the papillae of the gums, which cover a certain area of the tooth, there may also be mild bleeding of the gums and slight soreness;
- atrophic. It is characterized, as a rule, by the fact that the patient has an acute reaction to cold and hot food, while there is a decrease in the level of the gums and exposure of part of the tooth.
Treatment of gingivitis in the early stages can be both painless and quick if the patient follows all the doctor's instructions for oral hygiene. Sometimes curettage is required. The doctor will remove dental deposits either in a closed way, using special tools, or in an open way with cutting the gums.
With gingivitis of an infectious-inflammatory nature, the causative agent of the infection must first be eliminated. Antibacterial or antifungal agents are prescribed here. The chronic form of the disease requires treatment of the oral cavity with a solution of sodium bicarbonate, as well as anti-inflammatory drugs.
The presence of gingivitis often indicates a weakening of the immune system in the patient. In this regard, it is necessary to treat not only the inflammatory process, but also to increase the body's defenses. This will help the preparations of the group of immunocorrectors.
fungal diseases
Studies have found that almost fifty percent of the world's population are passive carriers of the Candida fungus. It can acquire activity under favorable conditions for it, especially when the patient's immunity is weakened. There are several types of candidiasis:
Thrush. The most common type. It is characterized, as a rule, by a white coating and dryness of the cheeks and lips from the inside, as well as on the back of the tongue and palate. These symptoms may be accompanied by a feeling of discomfort and burning, while small patients cope with thrush much easier than adults.
atrophic. It is believed that this type is the most painful. In the process of the development of the disease, the mucous membrane becomes dry, the oral cavity becomes bright red. Hyperplastic candidiasis is characterized by a large layer of plaque, if an attempt is made to remove it, then this ends with bleeding of the surface. In most cases, this type of fungal disease is caused by wearing a lamellar prosthesis for a long time, as a result of which the mucous membrane of the tongue, palate and corners of the mouth dries out with the further development of the inflammatory process. For the correct treatment of candidiasis, it is necessary to accurately establish its type, and this is possible only when conducting a whole range of tests.
Lichen planus. Also a fairly common type of fungal disease. It is characterized by the formation of ulcers, plaques and vesicles and redness in the patient's oral cavity. Quite often, lichen can be combined with gastric and hepatic disorders, diabetes.
Other diseases
In addition to the diseases that were mentioned above, there are a number of those that hardly belong to one or another group. As an example, the disease of the so-called geographical language can serve. This, as a rule, is not a dangerous pathology of the tongue, and it is difficult to call it a disease. It is characterized by covering the tongue with grooves that are somewhat similar to a geographical map.
However, among the diseases that cannot be classified, there are those that need attention. One of these diseases is oral dysbacteriosis. The factors that cause the development of the disease, in most cases, are the use of antiseptics and antibiotics to eliminate other causes during treatment.
Minor cracks in the corners of the lips, as well as loose teeth with damage to the enamel, can indicate the development of dysbacteriosis. To combat dysbacteriosis, it is necessary to restore the microflora of the oral mucosa.
Xerostomia. This disease is characterized by dryness, burning and inflammation of the oral mucosa. The reason for this is the disruption of the mucous and salivary glands, resulting in reduced secretion of mucus and saliva. In most cases, the disease manifests itself in patients who suffer from allergies, diabetes, and some other pathologies. Treatment is based on the elimination of provoking factors. In addition, the necessary sanitation of the oral cavity is carried out.
dental diseases
periodontal disease. As a result of the inflammatory process, dystrophy of all periodontal tissues is formed. Characteristic features is an anemic gum, you can see not only the neck, but the dental roots. Dental displacement and mobility of teeth are noted. In this case, patients do not experience pain. All this affects the timely appeal to a specialist, since the disease often has an imperceptible course. Which ultimately leads to the development of the following disease, which is discussed below.
Periodontitis. It is characterized by inflammation of the tissues that surround the teeth, mainly the gums and bones. Patients over forty years of age suffer from caries less than from this disease. And among those who have reached the age of sixty-five, according to studies, this disease develops in almost 80 percent. It was noted that men are less likely to suffer from periodontitis than women. The first symptom of the disease is gum bleeding, this can be observed both during cleaning and eating. Further signs may be accompanied by gingival swelling, as well as susceptibility to both cold and hot foods.
In most cases, the development of periodontitis is influenced by malocclusion, as a result of which a separate group of teeth experiences overload. By the way, more than 60 percent of the population suffers from this pathology. As the patient ages, systemic diseases can act as provoking factors, for example, in men it is ischemia, diabetes mellitus. The weaker half have hormonal disruptions during menopause, various problems associated with the thyroid gland.
In the course of treatment, first of all, it is necessary to take measures to remove plaque and dental deposits. Then treat the gums medicines that relieve inflammation. In almost one hundred percent of cases, antibiotics are used in the treatment of this disease. Often, patients are prescribed physiotherapy, for example, with the participation of a laser, which affects the inflammatory focus.
Surgical intervention is also practiced, especially in cases where tooth mobility occurs and there is a strong inflammation and tooth mobility. Through them, it becomes possible to carry out cleaning of dental deposits in hard-to-reach areas under the gum. For the purposes of prevention, it is necessary to take measures to correct the bite and try to avoid complications of chronic diseases that can provoke the development of periodontitis.
As mentioned at the beginning, these are only the most common diseases. There are enough of them. Some are not very complex in nature of inflammation, while others, on the contrary, pose a serious threat. The main thing is to identify the disease in time and take measures to treat it.
Finally
The disease of the oral cavity is a kind of mirror, which reflects the problems occurring inside the whole organism. Gastrointestinal disorders, various kinds of anemia and lack of vitamins in the body, weakened immunity, endocrine problems, allergies, and often more serious illnesses can provoke the development of the disease. In this regard, experts advise not to postpone a visit to the doctor if you suddenly find the presence of sores, blisters or redness in the oral cavity, regardless of whether they are painful or not. Only in this way can we hope for a quick and effective treatment.
In the dental department of the multidisciplinary medical center"Alternative" diagnostics and treatment a wide range diseases of the oral mucosa. These diseases are diverse, variable and cause a lot of suffering to patients, despite the fact that they can be correctly diagnosed and treated far from everywhere correctly, since this requires a good laboratory base and appropriate technical equipment.
Diseases of the oral mucosa (tongue, cheeks, lips) are a reflection of the internal problems of the whole organism. These diseases can be the result of problems with the gastrointestinal tract, various kinds of anemia and beriberi, endocrine problems, allergic reactions, and sometimes more serious and dangerous diseases. Therefore, if ulcers, blisters, redness have formed in the mouth, pain or burning is felt, contact your dentist immediately!
What refers to diseases of the oral mucosa?
- treatment of para- and hyperkeratosis using surgical methods;
- various forms of cheilitis and;
- vesicovascular diseases (vesicovascular syndrome, pemphigus);
- toxic-allergic lesions (erythema multiforme exudative);
- other diseases.
For a comprehensive diagnosis of diseases of the oral mucosa, the department conducts clinical and laboratory research methods, namely:
· General and biochemical blood tests, immunological tests of blood and saliva to assess the general condition of patients;
Screening and allergic reactions, hormonal status,
Microbiological examination of the microflora of the oral cavity - to determine the quantitative and qualitative assessment microorganisms;
PCR diagnostics of specific microflora both from lesions and interstitial diagnostics;
Identification of a specific infection - , RW, A, B, C;
· Cytological, morphological and cytomorphological research methods are used to diagnose pre-oncological and oncological conditions of the oral mucosa;
The most common diseases of the oral mucosa:
Stomatitis
- inflammation of the oral mucosa.
The symptoms of stomatitis are different in origin, but similar in essence - this is inflammation and extremely unpleasant sensations in the oral cavity, such as burning, dryness. Sometimes the disease is accompanied by fever.
Treatment of stomatitis is a process that must be approached very responsibly. First of all, it is necessary to eliminate the root cause of the disease, i.e. determine the cause of stomatitis and begin to eliminate it. To determine the cause of stomatitis, a therapist will help. Often they try to treat the disease on their own, using folk remedies. Remember that the treatment of stomatitis folk remedies, such as rinsing with soda several times a day will only help relieve symptoms, but will not relieve you of the disease, and stomatitis will reappear.
Medicine has advanced far in the treatment of this disease, so do not delay - contact the dentist-therapist of the clinic "Alternative"
GLOSSITIS
Inflammation of the mucous membrane of the tongue. Glossitis is more often superficial, that is, only the mucous membrane of the tongue becomes inflamed. But with deep injuries of the tongue (for example, a fish bone), purulent inflammation can develop in the thickness of the muscles with swelling of the tongue, impaired swallowing, and high body temperature; sometimes formed. Inflammation of the mucous membrane of the tongue often provokes the development of many diseases. More often, glossitis occurs in a catarrhal form: the tongue is slightly swollen, the mucous membrane is red, rawness and soreness are felt. Often a general examination of the patient is necessary to identify a disease of the internal organs that caused inflammation of the mucous membrane of the tongue. Therefore, it is important to contact the dentist in time, to fulfill all his appointments. Self-treatment is fraught with complications.
Desquamative glossitis ("geographic language", "migratory language").
It can be a symptom of various diseases, more often of the gastrointestinal tract, neurodystrophic processes, anemia, diabetes, allergic conditions. There is focal desquamation (removal of surface layers) of the epithelium of various sizes, whitish-gray in color with uneven borders. A rapid change in the outlines of the lesion is possible.
Treatment.
Medical glossitis.
Arises as allergic reaction after taking various drugs, more often antibiotics, sulfonamides, salicylates, etc. It is observed more often on the 4-7th day from the start of taking the drugs. Edema, redness, pronounced desquamation of the epithelium, a smooth, shiny surface appear on the tongue. The tongue may be somewhat thickened. Body temperature can rise to 38-38.5 °C. Characteristic common manifestations allergic reactions.
Treatment.
Cancellation of the drug or its replacement, desensitizing therapy, vitamins B, C, P, folic acid are carried out. Locally - anesthetics (rinses, applications). Sparing diet, plentiful drink.
Candida glossitis.
Occurs with the development of a secondary immunodeficiency state, with infection yeast-like fungi of the genus Candida.
Papillitis.
Inflammation of the papillae of the tongue. It occurs with injuries, infections, as a reactive state, with the pathology of the digestive system. The papillae of the tongue are edematous, enlarged, painful. Burning sensation in the affected area
Gingivitis
Gingivitis is an inflammation of the gums accompanied by swelling, redness and bleeding. Gingivitis is a fairly common disease; distinguish between acute, chronic and recurrent form of the disease.
Causes of gingivitis

The most common cause of gingivitis is non-compliance, resulting in the formation of (microorganism colonies firmly attached to the tooth surface). Also in the occurrence of gingivitis, factors such as pathology, tartar (calcified dental plaque), food debris, improperly applied or outdated, mouth breathing play a role.
Gingivitis is common in teenagers and pregnant women. In these categories of patients, the disease is usually more severe due to hormonal changes in the body.
Gingivitis can also be a sign of a systemic disease (eg, herpes, allergies, beriberi, leukopenia, wasting disease, diabetes mellitus).
Long-term use of certain drugs, such as oral contraceptives, can increase inflammation in the gums. Heavy metals (lead, bismuth) are also sometimes capable of provoking gingivitis.
Symptoms of gingivitis
With gingivitis inflames, arises, its contour changes. Due to edema, the gingival sulcus between the tooth deepens and the so-called. As a result, the following symptoms occur: reddening of the gingival margin, swelling and bleeding of the gums, the gums become sensitive and painful, there are difficulties in chewing and swallowing.
Chronic and acute gingivitis
Gingivitis can be either acute or chronic. Chronic gingivitis is most common in adults. During an exacerbation, which most often occurs in the winter-spring period, bleeding of the gums is noted (usually when brushing your teeth).
Treatment of gingivitis
Should only be done by a dentist. Treatment of gingivitis consists in the impact on dental plaques, the elimination of local and general predisposing factors.
First of all, you must carefully observe. The doctor will provide you with the necessary recommendations.
In addition, it is often necessary to resort to special means, and not only for the treatment of the acute phase of the disease, but also in order to slow down or stop the development of serious complications.
Various drugs are used: antibiotics, anti-inflammatory drugs, local immunocorrectors.
Sometimes significant medical intervention is required: thorough (mechanically or with the help of ultrasound), replacement and grinding of overhanging gums or ill-fitting ones.
In some cases it is necessary surgical intervention (curettage). During curettage, the doctor removes dental plaque using special hooks, excavators, curettes (closed curettage), or, if surgery is required, by cutting the gum (open curettage).
In chronic gingivitis, the mouth is treated with anti-inflammatory drugs and sodium bicarbonate solution.
With gingivitis caused by infectious and inflammatory processes, it is necessary to eliminate the causative agent of the infection. Therefore, the doctor may prescribe antibiotics or an antifungal drug.
Gingivitis often indicates a decrease in the body's own defenses. Therefore, treatment should be aimed not only at eliminating the inflammatory process, but also at increasing immunity. Then the use of immunocorrectors is most justified. Preparations of this group activate the defenses of the oral mucosa. Acting through a system of immunological mechanisms, they contribute to an increase in phagocytic activity (phagocytosis - the capture and neutralization of bacteria by cells immune system), an increase in the content of a special enzyme in saliva - lysozyme, known for its bactericidal activity, stimulation and an increase in the number of immunocompetent cells responsible for the production of antibodies.
To prevent gingivitis, the following simple rules must be followed:
Forecast
cheilite

X eilit - inflammation of the red border of the mucous membrane or skin of the lips. It can develop with trauma and cracks in the lips, due to burns, with prolonged exposure to the sun, frost - usually in windy weather.
Cheilitis angular infectious.
The disease is chronic, recurring, often found in children. It is caused by strepto-staphylococcal infection and fungi. The appearance of the disease is favored by reduced nutrition (lack of riboflavin), infectious foci in the oral cavity and nasopharynx,.
Clinical picture. Complaints of pain when opening the mouth. At the beginning of the disease, superficial erosion or cracks that quickly become infected. Eczematous phenomena can spread to the skin of the lips and chin adjacent to the corner of the mouth.
Cheilitis actinic.
Damage to the red border of the lips that occurs under the influence of prolonged exposure to the sun. Clinically, two forms are distinguished - exudative, which is characterized by puffiness and hyperemia, the appearance of bubbles, erosions, crusts, scales, cracks against this background; and dry (or xerotic), similar in clinical picture to the dry form of exfoliative cheilitis. The red border with this form of actinic cheilitis is bright red, covered with grayish-white scales, which reappear after their removal. Actinic cheilitis is characterized by relapses in the spring and summer.
Cheilitis apostematous.
The disease is predominantly lower lip. It is a type of glandular cheilitis.
clinical picture. The lip is edematous, hyperemic. Gaping holes are visible on the mucous membrane and the red border, from which drops of pus stand out. Dense nodules of hyperplastic small salivary glands are felt in the thickness of the mucous membrane.
Cheilitis ariboflavinous
often serves as a manifestation of deficiency in the body.
clinical picture. At the beginning of the disease, blanching of the mucous membrane and the red border of the lips, especially in the corners of the mouth, is observed, then exudative phenomena join, the epithelium macerates and exfoliates. The skin around the mouth opening is involved in the process. In the corners of the mouth, in place of the torn off epithelium, they form, covered with an easily removable crust of a yellowish color. Then the process extends to the red border and mucous membrane. Lips become bright red, vertical bleeding cracks appear. Burning in the oral cavity, hypersalivation, painful opening of the mouth are noted.
Cheilitis fungal
combined with a fungal infection of the oral mucosa, but can also occur in isolation on the red border of the lips, usually in the elderly. With prolonged existence, diffuse redness, peeling, slight swelling, and small cracks may develop on the skin of the lips. The picture resembles ordinary eczema.
Cheilitis is catarrhal.
Inflammation of the red border of the lip, which occurs under the influence of biological, mechanical, chemical, physical stimuli, sometimes due to damage during medical manipulations.
clinical picture. There are foci of hyperemia with subsequent destructive disorders in the form of erosion, ulcers. Characterized by edema, desquamation of the epithelium.
Cheilitis superficial purulent glandular
(cheilitis of Balti-Uina) is characterized by an extremely chronic course, painful inflammatory infiltration of the stroma around the small salivary glands, the formation of recurrent erosions and ulcers, and pyococcal infection of the labial glands.
Cheilitis penicillin
develops while taking penicillin. The red border of the lips is edematous, hyperemic, often noted. At the same time, penicillin stomatitis develops, which diffusely captures the mucous membrane of the soft and hard palate, lips, cheeks, tongue and manifests itself in the form of swelling, hyperemia. There is a burning sensation.
Cheilitis exfoliative.
Dysfunction of the thyroid gland plays a significant role in aggravating the disease. There are two forms - exudative and dry. With the exudative form, the lips are enlarged, the mouth is ajar due to sharp pain when the lips are closed. The lesion captures only the red border, sometimes moving to the mucous membrane of the lip. With a dry form of cheilitis in transition zone lips appear bands of congestive hyperemia, covered with thin transparent scales, after the removal of which a bright red surface with slight erosions is visible. The course is chronic.
Cheilitis eczematous.
The disease most often has an allergic nature. Allergens can be various microbes, chemicals (lipstick, medicinal substances).
clinical picture. The lip is hyperemic, edematous, dry with easily detachable scales, erosion, cracks, and crusts are possible.
Cheilitis treatment
The task of treating cheilitis at the dentist is to normalize the stereotype of lip closure. external sign physiological architectonics is the equality of the width of the actual red border of the upper and lower lips, i.e. closure - along the line delimiting the mucous membrane and the red border.
The complex of cheilitis therapy includes: a) normalization of nasal breathing by eliminating the habit of breathing through the mouth or by treating diseases of the nasopharynx; b) correction of bite anomalies; c) myotherapy to restore the normal tone of the circular muscle of the mouth.
Practice has shown that after breathing exercises the correct, complete closing of the lips spontaneously occurs, their architectonics is normalized. Therefore, the treatment of lip diseases should begin with the elimination of oral breathing, if any.
Oral diseases can have a variety of causes. These are problems with teeth, and diseases of internal organs, and damage (for example, hot or spicy food), and general dehydration, vitamin deficiency, as well as many other factors. All diseases that can occur in the human mouth can be divided into viral, infectious-inflammatory and fungal diseases. In addition, there are several unpleasant sores that cannot be attributed to any of these groups. In order to correctly choose a specialist to whom you need to contact with a particular problem, as well as in order to know which disease you can treat yourself and how, and which one cannot, you need to know each of the diseases of the mouth “by sight”.
Viral diseases
Viral diseases in the human oral cavity can cause herpes virus and human papillomavirus.
Herpes is one of the most common diseases. It is believed that ninety percent of people are infected with this virus.
An example of herpes on the lips.
Often this virus is located in the body in a latent form. In a strong person, it can manifest itself only as a small pimple on the lip, dying off without outside help within one to two weeks, while in a weakened person, herpes manifests itself much more significantly.
Calm herpes can be triggered "to action" by factors such as stress, surgery, colds, fever, lack of sleep, wind, cold, menstruation, immunosuppression.
Herpes develops, as a rule, in stages, passing through six stages. It all starts with itching and tingling on the lips and adjacent tissues, after which the lips swell, redden, soreness appears that interferes with eating and speaking, followed by the appearance of single vesicles or entire groups with vesicles. After a while, the blisters burst and turn into small ulcers. Ulcers are covered with a hard crust that can crack. In the final stage, the ulcers gradually disappear, redness and pain disappear.
At the first symptoms of herpes, ice should be applied to the lips and moistened with special balms. The bubbles that appear are lubricated with a special ointment that can be bought at a pharmacy without a prescription (for example, Penciclovir or Abreva). If a person is prone to too frequent exacerbations of herpes, then the doctor may prescribe antiviral drugs for him.
Papilloma
Papilloma in humans can occur in various parts of the body, but one type of human papillomavirus can cause the appearance of papillomas in the oral cavity. In the mouth, these sores look like cauliflower, that is, white plaques appear.
The most unpleasant consequences of this disease occur when it gets to the throat, because it can cause not only hoarseness, but also difficulty breathing.
Unfortunately, it is impossible to completely cure the human papillomavirus, so the treatment consists in eliminating the clinical manifestations. If we talk about the treatment of this virus in in general terms, then it comes down to choosing one of the methods: surgical, chemical, cytostatic, immunotherapy, or a combination of the above methods.
Infectious and inflammatory diseases
Infectious diseases of the oral cavity are the most common problem for which people turn to dentists, otolaryngologists or therapists. This species includes pharyngitis, gingivitis and.
Pharyngitis is an inflammation of the mucous membrane of the pharynx and, in particular, the throat. As a rule, it is accompanied by perspiration, discomfort and severe pain throat.

Acute pharyngitis.
Pharyngitis can provoke various factors: inhalation of cold or polluted air, tobacco smoke, various chemical pollutants. In addition, pharyngitis can also be caused by an infection (pneumococcus).
To the symptoms of pharyngitis already listed above (discomfort, sore throat and sore throat), you can also add general malaise, fever (the latter is typical only for acute pharyngitis, but not for chronic).
Diagnosed this disease general examination and throat swab. Doctors treat pharyngitis with antibiotics only in difficult cases, as a rule, only a special diet, hot foot baths, warm compresses on the neck, warm milk with honey, inhalations and rinses are enough.
Glossitis
Glossitis is an inflammatory process. It changes the structure as well as the color of the language. It is caused by oral infections. Glossitis can be provoked by a burn of the tongue, excessive love for hot drinks, injuries of the oral cavity and tongue, because all this is a kind of “pass” for infection. In addition, those who abuse alcohol, spicy foods and mouth fresheners are at risk. Of course, the chances of getting glossitis are also increased for those who neglect oral hygiene, in particular, use other people's toothbrushes.
The first symptoms of the disease are burning, discomfort, a little later, the color of the tongue becomes bright red, salivation increases. Further symptoms are dullness (or complete absence) of taste sensations. Although it is noticed that sometimes the sensation of tastes does not disappear, but is perverted.
If there is no treatment for this infection, the swelling of the tongue reaches such proportions that it becomes very difficult for a person to speak and eat, in addition, the tongue itself becomes covered with growths.
Treatment of glossitis is prescribed by a dentist. It consists in taking medications and a special diet based on semi-liquid food.
Gingivitis is characterized by inflammation of the lining of the gums. This is a fairly common disease that adolescents and pregnant women are most susceptible to.
Gingivitis affects the gums.
There are four types of this disease: catarrhal gingivitis, ulcerative necrotic, hypertrophic, atrophic.
- catarrhal gingivitis is characterized by symptoms such as redness and swelling of the gums, their itching and bleeding;
- with ulcerative necrotic gingivitis, ulcers and necrotic areas appear on the gums, in addition, the symptoms characteristic of this disease are bad breath, severe soreness, general weakness, fever and swollen lymph nodes;
- hypertrophic gingivitis enlarges the gingival papillae and covers part of the tooth with them, in addition, slight bleeding of the gums and mild soreness are possible;
- with atrophic gingivitis, a person begins to react sharply to hot and cold, the gum level decreases, and the tooth is exposed.
A dentist can treat gingivitis quickly and painlessly if treated early, and will also give oral hygiene advice to avoid this disease in the future.
Stomatitis
If we talk about infectious diseases of the oral cavity, then the most common of them is stomatitis.
Possible infection in the body different ways e.g. due to mechanical injury. After infection, a person develops special ulcers that are characteristic only for stomatitis. They are localized in inner surface cheeks and lips, at the root of the tongue, as well as under it. Have ulcers next view: shallow, single, round, smooth edges, and the center is covered with a film, as a rule, ulcers are very painful.
In the treatment of this disease, it is necessary to use special toothpastes and mouth rinses that do not contain sodium lauryl sulfate. To relieve the soreness of ulcers, anesthetics should be used. In addition, there are special drugs that help remove the harmful film from ulcers, which speeds up the treatment. And, of course, you can not do without anti-infection agents that the doctor will prescribe for you.
How to distinguish herpes from stomatitis?
Sometimes it is very easy to confuse the viral one that caused the infections, because in both cases painful wounds appear in the person's mouth. There are three characteristic differences between these diseases:
- herpes always appears in the same place, stomatitis always chooses new affected areas;
- herpes always affects those areas of tissue that are adjacent to the bones, stomatitis “likes” soft tissues more;
- during herpes, ulcers appear due to the bursting of small bubbles, and stomatitis initially begins with ulcers.
fungal diseases
Half the population the globe are inactive carriers of the Candida fungus. It can be activated if the body's immune defenses are weakened. Candidiasis (a disease caused by Candida) is of several types.
The most common is thrush. Its symptoms are dryness and white coating inside the cheeks and lips, on the palate and back of the tongue. All this is accompanied by a burning sensation and severe discomfort, and children tolerate thrush much easier than adults.
Most painful appearance candidiasis - atrophic. The mucous membrane of the oral cavity acquires a bright red color, becomes dry. With hyperplastic candidiasis, a thick layer of plaque appears, when you try to remove it, the surface begins to bleed.
This kind fungal disease, as atrophic candidiasis usually provokes prolonged wearing of lamellar prostheses. The mucous membrane of the tongue, palate and corners of the mouth dries up and becomes inflamed.
Treatment of the disease "candidiasis" can only be prescribed by a doctor, because it is extremely important to correctly determine its type, and for this you need to conduct a whole series of tests.
Lichen planus is another type of fungal disease. It causes plaques, blisters, ulcers and redness in a person's mouth. As a rule, lichen is combined with diseases such as diabetes, diseases of the stomach and liver.
Other diseases
In addition to the above diseases, there are several that are difficult to attribute to one or another group. For example, a geographical language, a completely harmless disease (although it is difficult to call it a disease, rather a change) of the language. In this case, the tongue is covered with a kind of grooves, reminiscent of a geographical map.
But among the unclassified diseases, there is one that is still worth paying attention to - this is oral dysbacteriosis. The cause of this disease is the intake of various antibiotics, antiseptics during the treatment of other problems.
Symptoms of dysbacteriosis begin with minor ones - cracks in the corners of the lips, bad smell from the mouth and reach the loosening of the teeth and damage to their enamel. To overcome dysbacteriosis, it is necessary to restore the healthy microflora of the oral mucosa.





